Rectocele
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a rectocele?
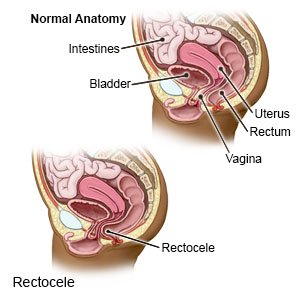
A rectocele happens when part of your rectum bulges into your vagina. This may happen if you have weak muscles and ligaments that cannot support the vagina and rectum. A wall of tough tissue, called the rectovaginal septum, separates the rectum from the vagina. The rectovaginal septum may be weak and thin. This allows part of the rectum to push into the vagina.
 |
What increases my risk for a rectocele?
- Pregnancy and childbirth
- Lower estrogen levels from older age or menopause
- Anything that strains your pelvic muscles, such as obesity, chronic constipation or straining during bowel movements, severe coughing, or lifting heavy objects
- Pressure in the pelvic area from a prolapsed bladder, rectum, or uterus
- A hysterectomy or other pelvic surgery
- Being born with weaker muscles in your rectum and vagina
What are the signs and symptoms of a rectocele?
- A soft bulge or lump in your vagina that may bulge through your vaginal opening
- Constipation or bowel movement that leaks out from your rectum
- Low back pain that goes away when you lie down
- Pain or pressure in your vagina when you urinate or have sex
- Pressure in your rectum, or you feel that your rectum is not empty after you have a bowel movement
How is a rectocele diagnosed?
Your healthcare provider will ask you about your lifestyle, past pregnancies, and any diseases you may have had. You may also need any of the following tests:
- A pelvic exam is used to check the size and location of a rectocele. Your provider will use a speculum to widen your vagina. Then you will strain or push down like you are having a bowel movement. You may need to tighten the muscles of your pelvis as if you are trying to stop urinating. This helps your provider learn the strength of your pelvic muscles.
- Defecography shows changes taking place in your rectum and muscles during a bowel movement. A thick paste of barium is placed into your rectum through your anus. X-rays are taken while you push out the barium as if you are having a bowel movement. The barium makes an x-ray outline of your rectum and anus.
- An MRI, ultrasound, or moving x-ray may be used to check your bowels, vagina, bladder, or rectum. You may be given contrast liquid to help the area show up better in pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. The MRI machine uses a powerful magnet. Do not enter the MRI room with anything metal. Metal can cause serious injury from the magnet. Tell the provider if you have any metal in or on your body.
- Anorectal manometry measures pressure in your anus an rectum. A flexible tube is inserted through your anus and into your rectum. Pressure is measured by sensors in the tube.
- Colonic transit studies measure how fast things pass through your colon. You will be asked to swallow a large pill containing plastic rings that serve as markers. The markers can be seen on x-rays. Pictures of your abdomen are taken for several days and the markers are counted. This helps your provider learn how long it takes for food to pass through your intestines.
Drugs used to treat this and similar conditions
Keflex
Keflex (cephalexin) is used to treat infections caused by bacteria, including respiratory ...
Cipro
Cipro (ciprofloxacin) is a fluoroquinolone antibiotic used to treat bacterial infections. Learn ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Botox
Botox is used to treat chronic migraines, excessive sweating, bladder conditions, eye muscle ...
Pyridium
Pyridium (phenazopyridine) treats pain, burning, increased urination, and increased urge to ...
Darifenacin
Darifenacin systemic is used for overactive bladder, urinary frequency, urinary incontinence
Sulfamethoxazole/trimethoprim
Sulfamethoxazole/trimethoprim systemic is used for acne, bacterial infection, bacterial skin ...
Hydroxyzine
Hydroxyzine is an antihistamine used to treat itching, hives, and anxiety. It also acts as a ...
Solifenacin
Solifenacin systemic is used for neurogenic bladder, neurogenic detrusor overactivity, overactive ...
How is a rectocele treated?
- Biofeedback therapy helps you learn to control and relax your pelvic muscles during a bowel movement. Ask your healthcare provider for more information about biofeedback.
- Estrogen is a hormone that may be taken as a pill, or applied as a vaginal cream. Estrogen helps keep your pelvic muscles strong and may prevent your rectocele from getting worse.
- A pessary is a plastic or rubber ring that is placed inside your vagina. This supports the bulging areas in your vagina and rectum.
- Surgery may be needed to move the rectum back into place. This surgery fixes the weak walls of your vagina.
How can I help prevent a rectocele?
- Do not strain. Do not lift heavy objects, stand for long periods of time, or strain to have a bowel movement. Prevent constipation by drinking plenty of liquids and eating foods high in fiber. Ask how much liquid to drink every day and which liquids are best for you. High-fiber foods, such as fruits, vegetables, and whole grains, soften bowel movements. This helps bowel movements pass more quickly through your colon. Slowly add fiber into your diet to avoid bloating, stomach pain, and gas.

- Do Kegel exercises regularly. These exercises can help your pelvic floor muscles get stronger. Tighten the muscles of your pelvis (the muscles you use to stop urinating). Hold the muscles tight for 5 seconds, then relax for 5 seconds. Gradually work up to holding the muscles for 10 seconds. Do at least 3 sets of 10 repetitions a day.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Your provider can help you create a weight loss plan, if needed. Your provider can also help you create a physical activity program. Physical activity, such as exercise, helps your bowels work better and decreases pressure inside your colon.
When should I seek immediate care?
- You have a mass bulging out of your vagina that you cannot push back into place.
- You vomit several times in a row.
- Your bowel movement is bright red or black.
When should I call my doctor?
- Your pain does not go away, even with treatment.
- Your pessary falls out.
- You have heavier vaginal bleeding than usual.
- You are unable to have a bowel movement.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
