Preeclampsia during Pregnancy
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is preeclampsia?
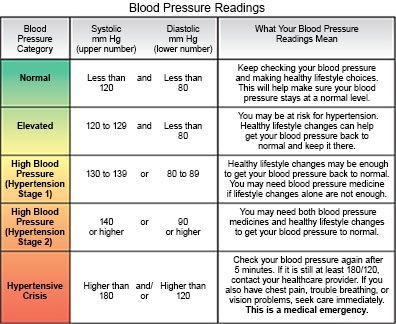
Preeclampsia is high blood pressure (BP) that usually develops after week 20 of pregnancy. It can also develop days or weeks after delivery. You may also have protein in your urine or damage to organs such as your kidneys or liver. Chronic hypertension with superimposed preeclampsia is preeclampsia in a woman with a history of hypertension before pregnancy. It can also be preeclampsia that develops before week 20 of pregnancy.
 |
What increases my risk for preeclampsia?
- Preeclampsia in a past pregnancy
- Being pregnant with more than 1 baby, or your first pregnancy
- Kidney disease, an autoimmune disease, diabetes, or chronic hypertension
- Age 35 years or older
- Being overweight
- A family history of preeclampsia
What are the signs and symptoms of preeclampsia?
- Swollen face and hands
- A sudden weight gain of 5 pounds or more
- Headache
- Spotted or blurred vision
- Pain in your upper abdomen
How is preeclampsia diagnosed?
Preeclampsia can lead to life-threatening conditions such as a stroke, eclampsia (seizures), or HELLP syndrome (blood cell destruction). It is important to get screened for high BP during pregnancy. High BP does not always cause symptoms. Symptoms that do develop may be general, such as headaches and swelling that you may think are not serious. Tell your healthcare provider if you had hypertension before you were pregnant. Also tell him or her about symptoms you are having, even if you think it is not serious.
- BP readings will be done regularly during your pregnancy. Preeclampsia means your BP is 140/90 or higher in 2 readings 4 hours apart. One or both numbers may be high. Your healthcare provider will also look at the results of your blood and urine tests.
- Blood tests are done to check your liver and kidney function. You may need blood tests every week while you are pregnant.
- Urine tests are used to check for protein. You may need to give healthcare providers a urine sample at each visit. You may also need to collect your urine every time you urinate for 24 hours. You may still have preeclampsia even if you do not have protein in your urine.
How is preeclampsia treated?
Treatment depends on how high your BP is and how many weeks you are into your pregnancy. Before 37 weeks, healthcare providers may want to monitor your condition if your BP is not severely high. The amount of amniotic fluid may be measured every week. Your provider will tell you how often to come in for tests. You may also need any of the following:
- An ultrasound may be done every 3 to 4 weeks to check your baby's growth.
- Medicines may be given to lower your blood pressure, protect your organs, or prevent seizures. You may be given steroid medicine to help your baby's lungs develop. These may be given if you have to deliver before 37 weeks of pregnancy. Low doses of aspirin after 12 weeks of pregnancy may be recommended if you are at high risk for preeclampsia. Aspirin may help prevent preeclampsia or problems that can happen from preeclampsia. Do not take aspirin unless directed by your healthcare provider.
- Delivery may stop preeclampsia. Healthcare providers may deliver your baby right away if he or she is full-term (37 weeks or more). He or she may need to be delivered early if you or the baby has life-threatening symptoms.
What can I do to manage preeclampsia during pregnancy?
Your BP will need to be checked by healthcare providers 1 to 2 times each week until your baby is born. The following are ways you can help manage high BP during pregnancy:
- Rest as directed. Your healthcare provider may tell you to rest more often if you have mild symptoms of preeclampsia. You may need to be in the hospital if your condition worsens.
- Do not drink alcohol or smoke. Alcohol, nicotine, and other chemicals in cigarettes and cigars, can increase your BP. They can also harm your baby. Ask your healthcare provider for information if you currently drink alcohol or smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Do kick counts as directed. You may need to keep track of how often your baby moves or kicks over a certain amount of time. Ask your obstetrician how to do kick counts and how often to do them.
- Check your weight each day. Weigh yourself every day before breakfast. Weight gain can be a sign of extra fluid in your body. Call your obstetrician if you have gained 2 or more pounds in a week.
Call your local emergency number (911 in the US) if:
- You have a seizure.
- You have chest pain.
When should I seek immediate care?
- You have severe abdominal pain with or without nausea and vomiting.
- You develop a severe headache that does not go away with medicine.
- You have blurred or spotted vision that does not go away.
- You are bleeding from your vagina.
When should I call my doctor or obstetrician?
- You have new or increased swelling in your face or hands.
- You are urinating little or not at all.
- You do not feel your baby's movements as often as usual.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Preeclampsia during Pregnancy
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
