POTS (Postural Orthostatic Tachycardia Syndrome)
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is postural orthostatic tachycardia syndrome (POTS)?
POTS is a term used to describe a fast heart rate that happens when you sit up or stand. Tachycardia is a heart rate of 100 beats per minute or more at rest. POTS may be caused by cardiovascular system problems, low blood volume, or blood pooling in your legs when you stand. A high level of certain hormones or health problems from another disease or condition can also cause POTS.
What increases my risk for POTS?
- Being female
- Puberty or pregnancy, due to hormone changes
- Major surgery or long-term bedrest
- A viral illness
- A disease or condition such as diabetes, Ehlers-Danlos syndrome, or Sjögren disease
- Low blood volume or a large blood loss
- An eating disorder, such as anorexia
What other signs and symptoms may happen with POTS?
You may have any of the following, depending on the cause:
- Chest pain
- Feeling lightheaded, dizzy, or faint
- Trouble standing or being physically active for long periods
- Headaches, neck pain, or blurred vision
- Trouble concentrating
- Fatigue or trouble sleeping
- Swelling in your legs or sweating in large amounts
- Nausea, vomiting, or abdominal pain
How is POTS diagnosed?
Your healthcare provider will examine you. Tell your provider about your symptoms and when they began. Include anything that makes your symptoms worse or better. Also tell your provider about any medicines you take or recent illness or surgery you had. Your provider will ask you to change positions while your heart rate and blood pressure are monitored. A drop in blood pressure within the first few minutes will rule out POTS. An increase in heart rate may mean you have POTS. Your provider may use any of the following to find the cause of your symptoms:
- Blood tests may be used to check your electrolyte level. Blood tests may also show if you have a condition such as anemia that may be causing your symptoms.
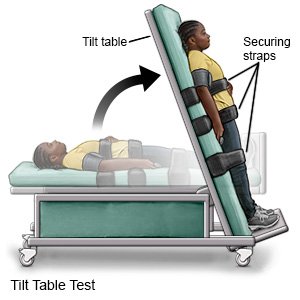
- A tilt table test may be used to confirm POTS. Your provider will put straps around your body to keep you in place. You will lie on a table and the table will move while your heart rate is checked.
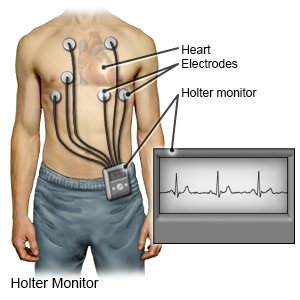
- A Holter monitor measures and records your heart's rate and rhythm over a period of time. A Holter monitor will show how fast your heart beats and if it beats in a regular pattern. You will wear it while you do your usual daily activities. A Holter monitor is usually used for 24 hours to check for symptoms of POTS.
- An EKG records the electrical activity of your heart. It is used to check for an abnormal heart rhythm.
- An echocardiogram (echo) is a type of ultrasound that shows the size and shape of your heart. An echo also checks how your heart moves when it is beating.
Drugs used to treat this and similar conditions
Lisdexamfetamine
Lisdexamfetamine systemic is used for ADHD, asperger syndrome, binge eating disorder, chronic ...
Armodafinil
Armodafinil may be used to improve wakefulness in adults who are very sleepy due to narcolepsy ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Duloxetine
Duloxetine is a selective serotonin and norepinephrine reuptake inhibitor antidepressant used to ...
Amantadine
Easy-to-read patient leaflet for amantadine. Includes indications, proper use, special ...
Amphetamine/dextroamphetamine
Amphetamine/dextroamphetamine systemic is used for ADHD, fatigue, narcolepsy
Methylphenidate
Methylphenidate is used to treat attention deficit disorder (ADD) and attention deficit ...
Dextroamphetamine
Dextroamphetamine systemic is used for ADHD, drowsiness, fatigue, narcolepsy, sexual dysfunction ...
Antivert
Antivert (meclizine) is used to treat or prevent nausea, vomiting, and dizziness caused by motion ...
Dramamine II
Dramamine II is used for motion sickness, nausea/vomiting, vertigo
How is POTS treated?
Treatment depends on the cause. Your healthcare provider will treat any medical condition causing your symptoms. Your provider may make changes to your current medicines if a medicine is causing your POTS. Lifestyle changes are usually recommended first. If lifestyle changes do not work, certain medicines may be recommended. No medicine is approved to treat POTS, but some medicines can treat underlying causes or symptoms. The goal is to use medicines to control symptoms so you can start an exercise plan. Medicines may be given to improve your heart rate or to increase your blood volume. Medicines may be given to improve energy and strength, or to control your immune system. You may also need medicines to prevent or treat nausea or pain.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to manage POTS?
Your healthcare provider will help you create a specific plan to manage POTS. The plan may include these and other guidelines:
- Know what to do if you feel your heart rate increase. Remember to sit up or stand up slowly to prevent symptoms. If you still feel symptoms when you change position, sit or lie back down right away. Your provider may also show you ways to bring your heart rate down. For example, you may be told to squeeze a rubber ball or to tighten certain muscles.
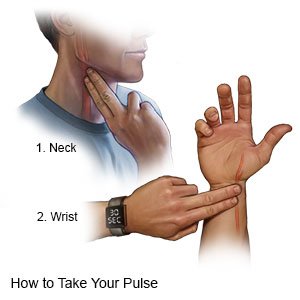
- Check your heart rate (pulse) as directed. Your provider will show you how to check your pulse, and how often to check it. Write down how fast your pulse is and what you were doing if your pulse is above 100. Bring the information with you to your follow-up appointments.
- Exercise as directed. Your provider or a physical therapist can show you how to exercise safely at home. Aerobic exercise, such as walking, can help strengthen your heart and lungs. Resistance training, such as lifting weights, can help build muscle strength. Your provider or therapist will tell you how much exercise to get each day, and which exercises are best for you. You might need to start with a few minutes of exercise at a time.
- Avoid heat. Heat can trigger your symptoms. Stay inside during very hot days, or limit the amount of time you are outside. Do not take hot baths or sit in a sauna.
- Control other medical conditions that can cause or worsen POTS. Your provider can help you create a management plan. You may also be referred to a specialist, such as a cardiologist.
- Wear compression stockings as directed. Compression stockings are tight around your lower legs. The pressure helps increase blood flow and reduce any swelling you may have in your legs.

- Make changes to the foods you eat, if needed. Have small, regular meals throughout the day. Your provider or a dietitian can help you create meal plans. You may also need to have more salt, depending on the cause of your POTS. Your provider or dietitian can help you get the right amount of salt each day. Other changes may be recommended if you have nausea, vomiting, or digestion problems.
- Drink more liquid, as directed. Liquid can help prevent or relieve some symptoms of POTS. For example, liquid can prevent you from getting too hot and triggering symptoms. Your provider will tell you how much liquid you need, and how often to drink liquid. Your provider will tell you which liquids are best for you. Limit or do not drink alcohol. Too much alcohol may trigger or worsen symptoms of POTS.
- Get more sleep, if needed. Sleep can help you feel less tired during the day. Sleep with an extra pillow or a folded blanket under your pillow to keep your head and upper body raised. This may help prevent you from becoming dizzy or lightheaded when you stand up in the morning.
Call your local emergency number (911 in the US) or have someone call if:
- You have trouble breathing.
- You collapse or go unconscious when you try to stand.
When should I seek immediate care?
- You cannot stand for 1 minute because your heart rate is very high, or you feel too lightheaded.
- You have severe pain.
- You have vomiting or diarrhea that is not stopping.
When should I call my doctor?
- You drink the recommended amount of liquid each day but are still having POTS symptoms.
- Your heart rate is higher than usual when you change position from lying to standing.
- Your brain fog or confusion is worse.
- You have muscle twitches.
- You cannot drink liquids as fast as you are sweating them out.
- Your lifestyle changes have made no change to your symptoms.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
