Patent Foramen Ovale
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a patent foramen ovale (PFO)?
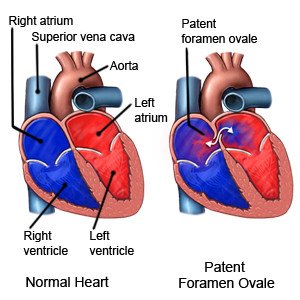
The foramen ovale is an opening between the right and left atria (the 2 upper chambers of the heart). The opening looks like a flap. All babies are born with a foramen ovale. The foramen ovale normally closes when the baby takes his or her first breath after being born. It should completely seal by the time a baby is 6 months to 1 year old. When it does not close and seal as it should, it is called a patent (open) foramen ovale. A PFO can last a few years or into adulthood. The cause of PFO is not known.
 |
What are the signs and symptoms of a PFO?
A small PFO usually does not cause any signs or symptoms. A larger PFO may cause any of the following:
- A stroke that has no clear cause
- Decompression sickness when you go SCUBA diving
- Migraine headache with aura
- Low oxygen levels that may cause bluish fingernails or lips in babies
How is a PFO diagnosed?
A PFO is often found during tests for other conditions. Your healthcare provider may want to check for a PFO if you had a stroke with no known cause. The stroke may be from a blood clot that traveled through the PFO and was pumped out to your brain. You may need any of the following:
- An echocardiogram is a type of ultrasound. Sound waves are used to form pictures of blood flow through the arteries of your heart. This test is called TTE if the sensor is placed on your chest or abdomen. It is called TEE if the sensor is placed down into your esophagus.
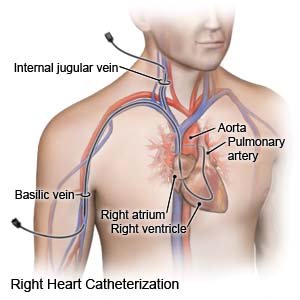
- Cardiac catheterization is a procedure to check how well your heart is working. It is also used to measure pressure in different parts of your heart. A tube is put into your heart through a blood vessel in your leg or arm. You may be given contrast liquid to help your heart show up better in pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A transcranial Doppler (TCD) measures how well blood flows through your brain's blood vessels. A TCD is used to check for a blood clot in a vessel.
How is a PFO treated?
A PFO that does not cause health problems usually does not need to be treated. A large PFO can cause a stroke, migraine headache, or other health problems. The following may be used to prevent a stroke or treat the PFO:
- Blood thinning medicine may be used to prevent blood clots. These medicines increase the risk for bleeding and bruising.
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Cardiac catheterization may be used as a procedure used to close the PFO through a catheter (thin tube). This procedure is used if you had a stroke. The catheter is placed into an artery in your groin and guided up to your heart. A device is then used to close the hole. This helps prevent another stroke caused by a blood clot.
- Surgery may be used to stitch the PFO closed.
What can I do to improve my heart health and help prevent a stroke?
If you had a stroke or are at risk for stroke or heart disease, healthcare providers will give you instructions. The following is general information:
- Prevent blood clots. Change your body position or move around often during the day. Move and stretch in your seat several times each hour if you travel by car or work at a desk. Move your legs by tightening and releasing your leg muscles while sitting. If you have to be on a long flight, get up and walk every hour. Drink water often during the flight.
- Maintain a healthy weight. Extra body weight can increase your risk for high blood pressure, diabetes, and coronary artery disease. Ask your healthcare provider what a healthy weight is for you. Ask your provider to help you create a weight loss plan, if needed.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart, blood vessel, and lung damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Limit or do not drink alcohol as directed. Alcohol can increase your risk for high blood pressure, diabetes, and coronary artery disease. Alcohol also increases your risk for a stroke. If you choose to drink alcohol, limit your daily and weekly amounts. In general, men should limit alcohol to 2 drinks per day. Women should limit alcohol to 1 drink per day. Limits depend on your age and heart health. Your provider will tell you if it is okay for you to drink alcohol, and how much is okay.
- Eat heart-healthy foods. Eat more fresh fruits and vegetables. Eat fewer canned and processed foods. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil. Other heart-healthy foods include walnuts, whole-grain breads, low-fat dairy products, beans, and lean meats. Fatty fish such as salmon and tuna are also heart healthy.

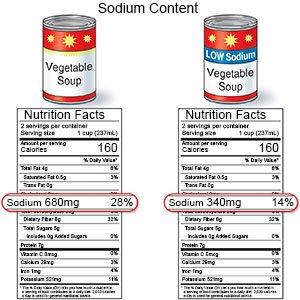
- Limit sodium (salt). Sodium can make your body retain (hold) extra fluid. Extra fluid makes your heart work harder. You may need to limit sodium to 2,300 milligrams (mg) each day. Your provider will tell you how much sodium is okay for you each day. A dietitian can help you create a meal plan that has the right amount of sodium.
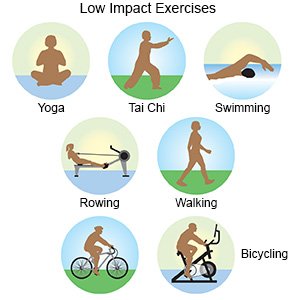
- Exercise regularly to help increase your blood flow. Walking is a good low-impact exercise. Talk to your provider about the best exercise plan for you. Ask your provider if you need to avoid strenuous activities. This is usually only needed if the PFO is causing symptoms.
Call your local emergency number (911 in the US) for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You cough up blood.
When should I seek immediate care?
- You are short of breath at rest or more short of breath than usual during exercise.
- Your lips or fingers are blue or white at rest.
- Your heart is beating faster than usual or fluttering more than usual.
- You feel dizzy or faint.
When should I call my doctor?
- You have swelling in your legs or ankles.
- You have severe abdominal pain or your abdomen is larger than usual.
- You have a fever.
- You have chills, a cough, or feel weak and achy.
- You feel depressed.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
