Open Cholecystectomy
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
What you need to know about open cholecystectomy:
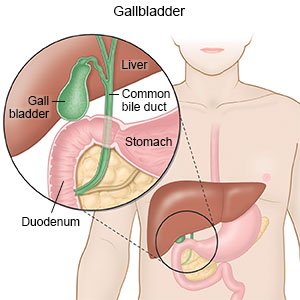
An open cholecystectomy is surgery to remove your gallbladder through an incision in your abdomen.
 |
How to prepare for open cholecystectomy:
- Your surgeon will tell you how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of surgery. Arrange to have someone drive you home after your surgery.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine before surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about all your allergies, including medicines, anesthesia, or antibiotics. Contrast liquid may be used during your surgery to help your surgeon see the gallbladder and bile duct better. Tell your surgeon if you have ever had an allergic reaction to contrast liquid.
- You may need to have chest x-rays, an ultrasound, or blood or urine tests. You may also need a liver and gallbladder scan or endoscopic retrograde cholangiopancreatography (ERCP).
What will happen during open cholecystectomy:
- You may be given antibiotic medicine through your IV to prevent infection. You will be given general anesthesia to keep you asleep and free from pain during the surgery.
- An incision will be made on your abdomen. Your healthcare provider will remove the gallbladder and tissues and blood vessels connected to it. He or she will check for bleeding and look for other problems in the area.
- A small tube called a drain may be placed to remove extra fluid from your abdomen. The incision will be closed with stitches and covered with a bandage.
What to expect after open cholecystectomy:
You may be taken to a recovery room until you are fully awake. Healthcare providers will watch you closely for problems. Do not get out of bed until your provider says it is okay. When your provider sees that you are okay, you will be taken back to your hospital room. The bandages covering your incision keep the area clean and dry to prevent infection. Your provider may remove the bandages soon after your surgery to check your incision.
- Medicines may be given to prevent or fight a bacterial infection, control pain, or prevent nausea. You may also be given medicine to help you have a bowel movement.
- Take deep breaths and cough 10 times each hour. This will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath, then let the air out and cough. Repeat these steps 10 times every hour.
- You may need to wear inflatable boots after surgery. The boots have an air pump that tightens and loosens different areas of the boots. This device improves blood flow and helps prevent clots.
- A nasogastric (NG) tube may be put into your nose and moved down your throat until it reaches your stomach. The tube will be attached to suction. Suction helps keep your stomach empty and also helps with nausea.
- A T-tube is a thin rubber tube that may be coming out of your abdomen after surgery. This tube drains bile onto a bandage or into a small bag.
Risks of open cholecystectomy:
The bile duct, nerves, blood vessels, muscles, and other organs near the gallbladder may be damaged. You may get an infection or bleed too much. Your signs and symptoms may not go away. You may get a blood clot in your leg or arm. This can be life-threatening.
Call your local emergency number (911 in the US) if:
- You feel lightheaded and have sudden shortness of breath.
- You have chest pain or cough up blood.
Drugs used to treat this and similar conditions
Tylenol
Tylenol is a pain reliever and a fever reducer used to treat many conditions such as headaches ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Dilaudid
Dilaudid (hydromorphone) is a narcotic pain reliever used to treat moderate to severe pain ...
Paracetamol
Paracetamol (Panadol, Calpol, Alvedon) is a widely used over-the-counter painkiller and fever ...
Qutenza
Qutenza patches are used to treat neuropathic pain associated with postherpetic neuralgia and ...
Acetaminophen/hydrocodone
The combination of hydrocodone and acetaminophen is used to relieve moderate to severe pain ...
Hydrocodone
Hydrocodone (Hysingla ER and Zohydro ER) is used for around-the-clock treatment of severe pain ...
Seek care immediately if:
- Your vomit looks like coffee grounds, or has blood in it.
- Your abdomen is severely painful and swollen.
Call your doctor or surgeon if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You feel full and cannot burp or vomit.
- Blood soaks through your bandage.
- Your incision is red, swollen, or has pus coming from it.
- Your stitches come apart.
- Your vomit is green.
- You have a fever.
- You have nausea and are vomiting.
- You are constipated or urinate less than usual.
- You have questions or concerns about your condition, surgery, or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics help prevent or fight an infection caused by bacteria.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
What to eat after surgery:
You may be given specific instructions for what to eat or not eat while you recover. The following are general guidelines:
- Eat low-fat foods for 4 to 6 weeks. This will help your body get used to digesting fat without a gallbladder. Slowly increase the amount of fat that you eat, as directed.
- Drink more liquids. Ask how much liquid to drink and which liquids are best for you.
Wound care:
- Keep the area clean and dry. Follow your provider's instructions on when you can bathe. Let water run gently over the area. Pat the area gently with a towel. Then put on a clean, new bandage as directed.
- Check for signs of infection. Look for redness, swelling, or pus each day. A fever is also a sign of infection.
Follow up with your doctor or surgeon as directed:
You may need to return to have your stitches removed. Your provider will check your incision for signs of infection. If you have a drain, he or she will remove it. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
