Non-Tunneled Central Lines
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a non-tunneled central line?
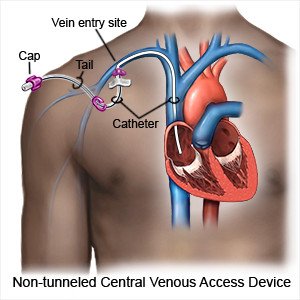
A non-tunneled central line is a type of short-term IV catheter. A non-tunneled central line may be put into a large vein near your neck, chest, or groin. Before you leave the hospital, you will be shown how to use, flush, and care for your central line. You will also be taught how to prevent an infection.
 |
Why may I need a non-tunneled central line?
Non-tunneled central lines are used to give you medicines and treatments. They are often put in if you have to give IV medicines to yourself at home. Healthcare providers may not be able to use smaller veins in your body. In an emergency, a non-tunneled central line gives easy access to your bloodstream, and medicine may work faster.
What do I need to remember about the central line?
The following can help prevent an infection or other problems:
- Clean and change the catheter parts as often as directed. You will be shown how to clean the caps, hubs, and injection ports. Always clean the parts before you attach and after you remove tubing from your catheter. Use a new alcohol pad for each part you clean. Throw away used alcohol pads. You may need to use extra tubing to get medicine. Ask your healthcare provider how often to change the caps and the medicine tubing.
- Clean and change the catheter parts as often as directed. You will be shown how to clean the caps, hubs, and injection ports. Always clean the parts before you attach and after you remove tubing from your catheter. Use a new alcohol pad for each part you clean. Ask your healthcare provider how often to change the caps and the medicine tubing.
- Flush your catheter before and after you use the central line. Your healthcare provider may give you syringes filled with saline (salt water) or heparin (a blood thinner) to flush your catheter. Stop if it is difficult to push the plunger. Do not force the saline or heparin into your catheter. This could damage the catheter or your vein. The force could also cause a blood clot to move into your blood. Stop when about 1 milliliter (mL) is left in the syringe. This will keep any air bubbles in the syringe.
- Clamp the catheter as needed. You may need to clamp your catheter at certain times, such as when the caps and tubing are being changed. The catheter is clamped to help prevent air from getting in.
- Loop and secure extra tubing. Loosely loop the tubing. Secure it to your arm with medical tape. This will help prevent the catheter from being pulled out by accident.
- Ask about activity. Your healthcare provider will tell you which activities are safe for you. You may not be able to play contact sports until the catheter is removed.
What can I do to prevent an infection?
The area around your catheter may get infected, or you may get an infection in your bloodstream. A bloodstream infection is called a central line-associated bloodstream infection (CLABSI). A CLABSI is caused by bacteria getting into your bloodstream through your catheter. This can lead to severe illness. The following are ways you can help prevent a CLABSI:
- Wash your hands often. Use soap or an alcohol-based hand rub to clean your hands. Clean your hands before and after you touch the catheter or the catheter site. Remind anyone who cares for your catheter to wash their hands.

- Limit contact with the catheter. Do not touch or handle your catheter unless you need to care for it. Do not pull, push on, or move the catheter when you clean your skin or change the dressing. Wear clean medical gloves when you touch your catheter or change dressings.
- Keep the area covered and dry. Keep a sterile dressing over the catheter site. Wrap the insertion site with plastic and seal it with medical tape before you bathe. Take showers instead of baths. Do not swim or soak in a hot tub.
Call your local emergency number (911 in the US) for any of the following:
- You have pain in your arm, neck, shoulder, or chest.
- You cough up blood.
- You have chest pain or trouble breathing.
When should I seek immediate care?
- The catheter site is cold, changes color, or you cannot feel it.
- You see blisters on the skin near the catheter site.
When should I call my doctor?
- You have a fever.
- The catheter site is red, warm, painful, or is oozing fluid.
- You see blood on your bandage and the amount is increasing.
- The veins in your neck or chest bulge.
- You cannot flush your catheter, or you feel pain when you flush your catheter.
- You see that the catheter is getting shorter, or it falls out.
- You see a hole or a crack in your catheter. Clamp your catheter above the damage before you call your doctor.
- You have questions about how to care for your catheter.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
