The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Laparoscopic Burch Procedure
Medically reviewed by Drugs.com. Last updated on Feb 20, 2025.
WHAT YOU SHOULD KNOW:
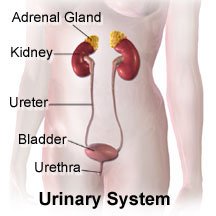
- A laparoscopic Burch procedure is also known as urinary bladder suspension. This procedure is done to treat stress urinary incontinence and bladder prolapse. Stress urinary incontinence is a condition where urine leaks before you are able to reach the toilet. This is due to sudden extra pressure put on the bladder. Small amounts of urine may escape during activities, such as laughing, coughing, and sports. A bladder prolapse happens when the ligaments supporting the bladder become weak. This causes the bladder to protrude or extend into the vagina.
- In a laparoscopic Burch procedure, small incisions (cuts) are made around the belly button. Caregivers will insert special tools and a laparoscope through these incisions to do the procedure. A laparoscope is a long metal tube with a light and magnifying glass on the end. During this procedure, the bladder will be pulled up into a more fixed position. Sutures (threads) are used to tie the neck of the bladder on each side to a strong ligament. This procedure will prevent the bladder from moving down, and urine from leaking during activities.
INSTRUCTIONS:
Medicines:
- Keep a current list of your medicines: Include the amounts, and when, how, and why you take them. Take the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency. Throw away old medicine lists. Use vitamins, herbs, or food supplements only as directed.
- Take your medicine as directed: Call your primary healthcare provider if you think your medicine is not working as expected. Tell him about any medicine allergies, and if you want to quit taking or change your medicine.
- Antibiotics: This medicine is given to fight or prevent an infection caused by bacteria. Always take your antibiotics exactly as ordered by your primary healthcare provider. Do not stop taking your medicine unless directed by your primary healthcare provider. Never save antibiotics or take leftover antibiotics that were given to you for another illness.
- Pain medicine: You may need medicine to take away or decrease pain.
- Learn how to take your medicine. Ask what medicine and how much you should take. Be sure you know how, when, and how often to take it.
- Do not wait until the pain is severe before you take your medicine. Tell caregivers if your pain does not decrease.
- Pain medicine can make you dizzy or sleepy. Prevent falls by calling someone when you get out of bed or if you need help.
Ask for information about where and when to go for follow-up visits:
For continuing care, treatments, or home services, ask for more information.
Activity:
- Ask your caregiver about doing Kegel exercises: These exercises squeeze your pelvic floor muscles and help them become stronger. Ask your caregiver when to start doing these exercises.
- Avoid too much pressure in your abdomen (stomach): Do not strain, lift heavy objects, or stand for a very long time. Do not perform hard exercise, such as running and weight lifting.
- Begin walking as soon as possible: Do not stay in bed for too long. Caregivers may have you start walking within a few hours after the procedure.
Drugs used to treat this and similar conditions
Myrbetriq
Myrbetriq (mirabegron) is used to treat overactive bladder with symptoms of frequent or urgent ...
Oxybutynin
Oxybutynin is used to treat symptoms of overactive bladder such as incontinence. Learn about side ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Botox
Botox is used to treat chronic migraines, excessive sweating, bladder conditions, eye muscle ...
VESIcare
Vesicare is used to treat symptoms of overactive bladder such as incontinence and frequent ...
Tofranil
Tofranil is used for depression, enuresis, pain, primary nocturnal enuresis
Toviaz
Toviaz (fesoterodine) is used to treat overactive bladder with symptoms of urinary frequency ...
Amitriptyline
Amitriptyline is a tricyclic antidepressant used to treat depression and, off-label, conditions ...
Mirabegron
Mirabegron systemic is used for neurogenic detrusor overactivity, overactive bladder, urinary ...
Foley catheter:
Your caregiver may ask you to insert a Foley catheter on your own. A foley catheter is a tube that is put into your bladder to drain your urine into a bag. The bladder is an organ where urine is kept. The catheter may make you feel like you have to urinate. If you are able to relax, the catheter will drain the urine for you. When the catheter is taken out, you can urinate on your own. Ask your caregiver for more information about self-catheterization.
- Do not pull on the catheter because this will make you hurt or bleed.
- Do not kink the catheter because the urine will not be able to drain out.
- Do not lift the bag of urine above your waist. If you do this the urine will flow back into your bladder, and may cause an infection.
Manage your stress:
Stress may slow healing and lead to illness. Learn ways to control stress, such as relaxation, deep breathing, and music. Talk to someone about things that upset you.
Wound care:
When you are allowed to bathe or shower, carefully wash the incisions (cuts) with soap and water. Afterwards, put on clean, new bandages. Change your bandages any time they get wet or dirty. Ask your caregivers for more information about wound care.
CONTACT A CAREGIVER IF:
- Your bandage becomes soaked with blood.
- You have a fever.
- You have chills, a cough, or feel weak and achy.
- You have nausea (upset stomach) or vomiting (throwing up).
- You have discharge or pain in the area where the urine catheter was inserted.
- You have chest pain or trouble breathing that is getting worse over time.
- You have questions or concerns about your procedure, illness, or medicine.
- You are urinating less often than you usually do.
SEEK CARE IMMEDIATELY IF:
- You have any of the following problems:
- Blood is present in your urine or catheter.
- Pain when passing urine or having sex.
- You have pain in the abdomen (stomach) that does not go away even after taking pain medicines.
- Your incisions have pus or a foul-smelling odor.
- You suddenly feel lightheaded and have trouble breathing.
- You have new and sudden chest pain. You may have more pain when you take deep breaths or cough. You may cough up blood.
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
