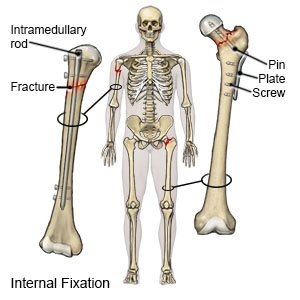
Intramedullary Nailing
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
Intramedullary nailing is surgery to repair a broken bone and keep it stable. You may have a little bleeding from the wound for the first 24 hours after surgery. Stitches or staples used to close the surgery wound may be removed about 14 days after surgery.
 |
DISCHARGE INSTRUCTIONS:
Call 911 for any of the following:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Seek care immediately if:
- You have severe pain that increases when you stretch or bend the area.
- Your skin is swollen, tight, or hard. It may be pale or shiny. The area may also be numb and hard to move.
- Your wound is red, swollen, or draining pus.
- You wound has a foul odor.
- Your stitches or staples come apart.
Contact your healthcare provider if:
- You have a fever or chills.
- You have nausea or vomiting.
- Your skin is itchy, swollen, or you have a rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take pain medicine safely.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Antibiotics may be given to help prevent or fight a bacterial infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for your wound
by keeping it clean and dry. Keep the wound dry when you shower. Cover the wound with a plastic bag. Tape the bag to your skin above the wound. Check your wound daily for signs of infection, such as redness, pus, or swelling.
Drugs used to treat this and similar conditions
Prolia
Prolia (denosumab) is an injection that is administered subcutaneously (under the skin) once every ...
Fosamax
Fosamax (alendronate) is used to treat or prevent postmenopausal osteoporosis and steroid-induced ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Forteo
Forteo injection is used to treat osteoporosis in men and postmenopausal women who are at high risk ...
Evenity
Evenity (romosozumab) injection is used to treat osteoporosis in postmenopausal women to reduce the ...
Tymlos
Tymlos (abaloparatide) is used to treat osteoporosis in men and postmenopausal women who have a ...
Romosozumab
Romosozumab is used to treat osteoporosis in postmenopausal women at high risk of fractures. It is ...
Calcium carbonate
Calcium carbonate systemic is used for duodenal ulcer, erosive esophagitis, GERD, hypocalcemia ...
Teriparatide
Teriparatide systemic is used for hypoparathyroidism, osteoporosis
Go to physical therapy
as directed. A physical therapist can teach you exercises to help strength your bones.
Apply ice
over the surgery area for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel. Ice helps prevent tissue damage and decreases swelling and pain.
Elevate
your leg or arm above the level of your heart as often as you can. This will help decrease swelling and pain. Prop your arm or leg on pillows to keep it elevated comfortably.
Wear a compression stocking
as directed. This is a long, tight stocking that puts pressure on your leg to increase blood flow and prevent blood clots. You may need to wear the stocking all day. Your healthcare provider may tell you to continue wearing the stocking for several months after surgery.
 |
Eat a variety of healthy foods
every day. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Your healthcare provider may recommend that you get more calcium and vitamin D. Calcium and vitamin D work together to strengthen bone. Your healthcare provider or a dietitian can help you create a meal plan.
Follow up with your healthcare provider as directed:
You may need to have x-rays over the first 6 months after surgery to make sure the fracture is healing. The locking screws may be removed after the bone heals. The nail is usually not removed. Tell your healthcare provider if you feel irritation or pain where the nail was placed. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
