Iliac Vein Compression Syndrome
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is iliac vein compression syndrome (IVCS)?
IVCS is a condition that affects the blood flow in a vein near your pelvis. The vein gets compressed by another structure in your body such as an artery or vertebrae. This closes the vein and stops blood flow from your leg to your heart. IVCS is also known as May-Thurner syndrome.
What are the signs and symptoms of IVCS?
You may only develop symptoms if you have poor blood flow for a long period of time or develop a blood clot. Symptoms usually only affect one leg:
- Pain, tenderness, or swelling
- Skin color changes or open sores
- Large, twisted, and swollen veins (varicose veins)
- Heaviness, tiredness, or cramping
How is IVCS diagnosed?
IVCS may be found during an imaging test for another reason. Tell your healthcare provider about any symptoms you have and when they started. You may need any of the following:
- Doppler ultrasound is used to check the blood flow in your vein. Doppler is also used to check if you have a blood clot.
- CT or MRI venography will show if your blood vessel is compressed or if you have a blood clot. You will be given contrast liquid to help the blood vessels show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. The MRI machine uses a powerful magnet. Metal can cause serious injury from the magnet. Tell the healthcare provider if you have any metal in or on your body.
How is IVCS treated?
Treatment depends on your symptoms and if you have a blood clot. You may need any of the following:
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
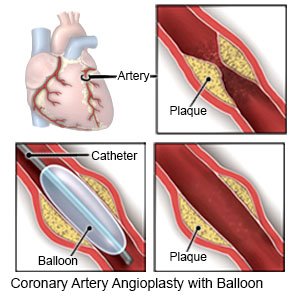
- Angioplasty is a procedure to open your vein so blood can flow through properly. A catheter (thin tube) is used to insert a balloon into the vein. The balloon is inflated to open the vein and is then removed. A stent (small metal mesh tube) may be placed to help keep the vein open.
- Thrombolysis is a procedure to break up a clot. Medicine is injected into the vein to help break the clot apart.
- Thrombectomy is surgery to remove a clot.
Drugs used to treat this and similar conditions
Xarelto
Xarelto (rivaroxaban) is a factor Xa inhibitor used to reduce the risk of blood clots and stroke in ...
Eliquis
Eliquis (apixaban) is used to reduce the risk of stroke and systemic embolism in patients with ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Lovenox
Lovenox is used to prevent deep vein thrombosis (DVT) which can lead to blood clots in the lungs ...
Coumadin
Coumadin is used to prevent heart attacks, strokes, and blood clots in veins and arteries. Learn ...
Heparin Sodium
Heparin Sodium is used for angina, anticoagulation during pregnancy, antiphospholipid syndrome ...
Alteplase
Alteplase systemic is used for heart attack, ischemic stroke, IV Catheter Clot, pulmonary embolism ...
Argatroban
Argatroban systemic is used for thrombotic/thromboembolic disorder
Enoxaparin
Enoxaparin systemic is used for acute coronary syndrome, angina, deep vein thrombosis, deep vein ...
How can I manage my symptoms?
- Wear a compression device as directed. Examples include pressure stockings, intermittent pneumatic compression, and sequential compression devices. A compression device puts pressure on your lower legs to help keep blood from pooling in your leg veins. Your healthcare provider can prescribe the right device for you. Do not buy over-the-counter devices unless your provider says it is okay. They may not fit correctly or may have elastic that cuts off your circulation. Ask your provider when to start wearing a compression device and how long to wear it.

- Elevate your legs above the level of your heart. Elevate your legs when you sit or lie down, as often as you can. This will help decrease swelling and pain. Prop your legs on pillows or blankets to keep them elevated comfortably.

- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You have trouble breathing.
When should I seek immediate care?
- Your leg feels warm, tender, and painful. It may look swollen and red.
- You have pain in your leg that does not go away or gets worse.
- Your leg is swollen and hard.
When should I call my doctor?
- You have painful varicose veins.
- You have new or worsening leg pain, swelling, or redness.
- You have new or worsening ulcers or other sores on your leg.
- Your symptoms keep you from doing your daily activities.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
