Hypertension during Pregnancy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about hypertension during pregnancy:
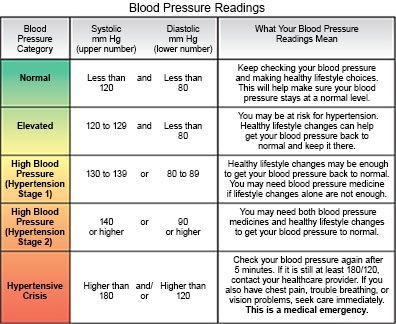
Hypertension is high blood pressure (BP). Normal BP is 119/79 or lower. Hypertension during pregnancy is a BP of 140/90 or higher. Severe hypertension is 160/110 or higher. One or both numbers of these readings may be high. Hypertension may start before you become pregnant, or develop during pregnancy. Pregnancy can cause high BP, or it may develop because of other risk factors you had before you became pregnant. It is important to get screened and treated for an elevated BP or hypertension during pregnancy. This can prevent problems for you and your baby.
 |
Types of hypertension during pregnancy:
- Chronic hypertension is high BP that starts before pregnancy or develops within the first 20 weeks and does not go away after delivery.
- Gestational hypertension means you develop new high BP after week 20 of your pregnancy. Gestational hypertension usually goes away after delivery, but it increases your risk for future chronic hypertension or heart disease.
- Chronic hypertension with superimposed preeclampsia is preeclampsia in a woman with a history of hypertension before pregnancy. It can also be preeclampsia that develops before week 20 of pregnancy.
- Preeclampsia is high BP that usually develops after week 20 of pregnancy. It can also develop within 4 weeks of delivery. You may also have protein in your urine or damage to organs such as your kidneys or liver. Preeclampsia can lead to life-threatening conditions such as a stroke or eclampsia (seizures from severe high BP).
- HELLP syndrome is a life-threatening complication of high BP that may develop between week 20 of pregnancy and a few days after delivery. It causes destruction of red blood cells, liver problems, and blood clotting problems. Your risk for HELLP syndrome increases if you have a history of preeclampsia.
Signs and symptoms
do not always happen with high BP. Hypertension may only be found during routine pregnancy checkups. You may have any of the following, depending on the kind of hypertension you have:
- Headache or confusion
- Spotted or blurred vision
- Chest pain, trouble breathing, or a fast heartbeat
- Dizziness or weakness
- Abdominal pain, or pain on the right side of your upper abdomen, behind the ribs
- Nausea and vomiting
- Ringing or buzzing in your ears
- Sudden weight gain or swelling in your face, arms, or legs
- Severe fatigue that does not get better with rest
Call your local emergency number (911 in the US), or have someone else call if:
- You have a seizure.
- You have chest pain.
- You faint or lose consciousness.
- You have trouble breathing.
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
Seek care immediately if:
- You have a severe headache or vision loss.
- You have weakness in an arm or leg.
- You urinate less than usual or stop urinating.
- You have fluid or blood leaking from your vagina that does not stop.
- You feel a gush of fluid from your vagina.
- You have severe abdominal pain with or without nausea and vomiting.
- You feel a change in your baby's movement, or you feel fewer than 6 to 10 movements in an hour.
Call your doctor or obstetrician if:
- You have new or increased swelling in your face or hands, or sudden weight gain.
- You have questions or concerns about your condition or care.
How hypertension during pregnancy is diagnosed and treated:
Your healthcare provider will check for hypertension at each prenatal visit. Your provider will check your BP and ask if you have any symptoms of hypertension. You may need blood or urine tests to check for problems caused by hypertension. Treatment depends on how high your BP is and how many weeks you are into your pregnancy. Before 37 weeks, healthcare providers may want to monitor your condition if your BP is not severely high. An ultrasound may be done every 3 to 4 weeks to check your baby's growth. The amount of amniotic fluid may be measured every week. Your provider will tell you how often to come in for tests. Treatment may include any of the following:
- Medicine may be given to lower your BP or prevent seizures. The dose of current BP medicine you take may need to be changed. Daily low-dose aspirin may be recommended if you are at high risk for preeclampsia. Aspirin may help prevent preeclampsia or problems that it can cause. Your healthcare provider will tell you if you should take aspirin, and when to start. It is usually recommended from week 12 of pregnancy until delivery. Do not take aspirin unless directed by your healthcare provider.
- Ultrasounds are used to check your baby's growth and make sure he or she is healthy.
- Delivery may be recommended. Delivery may stop high BP or problems such as preeclampsia. Healthcare providers may deliver your baby right away if he or she is full-term (37 weeks or more). You may need to deliver your baby early if you or the baby has life-threatening symptoms.
Manage hypertension during pregnancy:
Your healthcare providers will tell you what BP is best for you during your pregnancy. They will help you create a plan to lower your BP safely and keep it at recommended levels. This is based on the kind of hypertension you have and how high your BP is. Sometimes it is difficult to diagnose a specific kind of hypertension, but you can still follow general guidelines:
- Go to all scheduled appointments. Your healthcare providers will check your blood pressure and may order other tests.
- Rest as directed. Your healthcare provider may tell you to rest more often if you have mild symptoms of preeclampsia.
- Check your BP as directed if you have chronic hypertension. Sit and rest for 5 minutes before you take your BP. Extend your arm and support it on a flat surface. Your arm should be at the same level as your heart. Follow the directions that came with your BP monitor. Take your BP as often as directed. Keep a record of your BP readings and bring it to your follow-up visits.

- Do not drink alcohol or smoke. Alcohol, nicotine, and other chemicals in cigarettes and cigars can increase your BP. They can also harm your baby. Ask your healthcare provider for information if you currently drink alcohol or smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Eat healthy foods. Healthy foods can help control your BP. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if you need to be on a special diet.

- Exercise if directed. Exercise can help lower your BP. Ask your healthcare provider how much exercise you need and which exercise is right for you.
- Do kick counts as directed. You may need to keep track of how often your baby moves or kicks over a certain amount of time. Ask your obstetrician how to do kick counts and how often to do them.
- Check your weight each day. Weigh yourself every day before breakfast. Weight gain can be a sign of extra fluid in your body.
Follow up with your doctor or obstetrician as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
