Formula Intolerance
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is formula intolerance?
Formula intolerance means your baby has trouble digesting formula. He or she may be sensitive to an ingredient in the formula. Intolerance is different from an allergy. An allergy means your baby's immune system reacts to a protein in the formula and can be life-threatening. Intolerance means it causes irritation in your baby's digestive system. Intolerance is not life-threatening, but it may lead to dehydration or failure to thrive. Failure to thrive means your baby does not gain weight or grow as fast as he or she should.
What are the signs of formula intolerance?
- Diarrhea
- Blood or mucus in your baby's bowel movements
- Vomiting
- Pulling his or her legs up toward the abdomen because of abdominal pain
- Colic that makes your baby cry constantly
- Trouble gaining weight, or weight loss
How is formula intolerance diagnosed and treated?
- Your baby's pediatrician will examine your baby. He or she will ask about your baby's reaction to formula and when it started. Tell him or her which formula you use. The pediatrician may take a sample of your baby's bowel movement. The sample will be tested to rule out other health problems your baby may have. Your baby may also need tests to find if he or she has an allergy to a protein in the formula.
- A change of formula may be the only treatment your baby needs. Signs of intolerance may go away on their own after the change. Your baby may need to have treatment for health problems caused by intolerance.
How is formula intolerance treated?
- Change your baby's formula if directed. Formula may be made with cow's milk, soy, or rice protein. Your baby may need a hypoallergenic formula if he or she cannot have any of these kinds of formula. These proteins are broken down, so your baby can digest them more easily. Your baby's pediatrician will tell you which formula to use. You may need to try a few to find what works best for your baby. You may need to mix a new formula with the current formula at first. This will help your baby get used to the taste of the new formula. You will start increasing the amount of new formula over time. Your baby's pediatrician will explain how to do this. You will need to watch for signs of intolerance as your baby gets more of the new formula.
- Ask about breastfeeding, if possible. You may be using formula because your breasts do not make enough milk. You may also be having problems such as sore nipples or plugged ducts. Healthcare providers and lactation consultants may be able to help you. Breastfeeding can help soothe and comfort your baby. It can also help him or her get liquids and the nutrition he or she needs. You may be able to pump your breasts and give the milk to your baby in a bottle. If you are going to give your baby breast milk, you may need to avoid cow's milk, soy, or other foods causing your baby's condition. These proteins may be passed through your breast milk.
- Ask about an oral rehydration solution (ORS) to treat or prevent dehydration. Your baby can become dehydrated from vomiting, diarrhea, or low formula intake. An ORS is a drink that contains salt, sugar, and minerals to replace body fluids. Your baby's pediatrician can tell you which kind of infant ORS to get and how much to give your baby. Use a syringe to give your baby the ORS. An ORS is usually given in small amounts (about 1 teaspoon at a time) if your baby has been vomiting. If your baby vomits after you give the ORS, wait 30 minutes and try again. Do not give your baby fruit juices or sports drinks. Fruit juices can make his or her condition worse. A sports drink is not the same as an ORS.
What can I do to comfort my baby?
Formula intolerance can cause your baby to spit up or be fussy. The following can help him or her feel better:
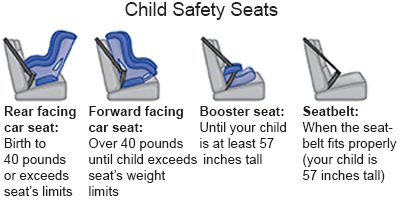
- Help soothe your baby's stomach and relieve gas with motion. After a feeding, walk around while you hold your baby. You can also try sitting in a rocking chair, or putting your baby in a baby swing. Your baby may be soothed by a ride in the car. Always put your baby in a rear-facing car seat.
- Burp your baby often during feedings. You may need to burp him or her more often than usual if he or she is fussy.
- Rub your baby's back. This can help calm your baby and relieve gas. Lay your baby across your lap with his or her stomach on your legs to create pressure. Gently and slowly rub your baby's back. Do not put your baby to bed on his or her stomach. Always lay your baby on his or her back to sleep.

- Play sounds to calm or soothe your baby. Music or a white noise machine may help if your baby is crying. You can also set your baby safely near a dishwasher or clothes dryer.
- Feed your baby less formula more often. Give your baby less formula at a feeding. Be sure to increase the number of feedings during the day. This will help prevent dehydration and malnutrition.
- Let your baby rest and digest the formula after a feeding. A little motion is okay and may be soothing, but be gentle. Do not bounce or play with your baby right after a feeding.
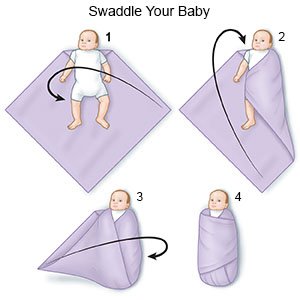
- Swaddle him or her snugly in a light blanket. Your baby's pediatrician can show you how to swaddle him or her.
What else can I do to care for my baby?
- Do not use a microwave to heat your baby's formula. The formula will not heat evenly and will have spots that are very hot. Your baby's face or mouth could be burned. You can warm formula quickly by placing the bottle in a pot of warm water for a few minutes.
- Be careful not to overfeed your baby. Overfeeding means you try to get your baby to keep feeding when he or she is done. Overfeeding can happen when you find a formula your baby can tolerate. Do not try to give your baby extra formula to make up for weight loss unless directed. Overfeeding can also happen if you add baby cereal to the formula. You can make more formula if your baby is still hungry after he or she finishes a bottle.
- Always hold your baby upright during feedings. Do not let your baby lie flat during a feeding. Hold the bottle for your baby. Do not prop a bottle in your baby's mouth or let him or her sleep with a bottle. He or she may choke. The milk may also flow into his or her middle ear and cause an infection. If he or she falls asleep while drinking, the milk will pool around his or her teeth and may cause tooth decay.
When should I call my baby's pediatrician?
- Your baby has a fever.
- Your baby has vomited more than 2 times in the past 24 hours.
- Your baby has had more than 5 episodes of diarrhea in the past 24 hours.
- Your baby has a new or worsening rash.
- Your baby has new or worsening breathing problems.
- Your baby is very irritable and cannot be consoled.
- Your baby has signs of dehydration, such as a soft spot that is sunken. He or she may cry without tears, have sunken eyes, or a dry mouth.
- Your baby is 4 or more days old and has fewer than 6 wet diapers each day.
- Your baby is 4 or more days old and has fewer than 3 bowel movements each day.
- Your baby is weak and sleeping more than usual.
- You have questions or concerns about your baby's condition or care.
Care Agreement
You have the right to help plan your baby's care. Learn about your baby's health condition and how it may be treated. Discuss treatment options with your baby's healthcare providers to decide what care you want for your baby. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
