Enterocele Repair
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
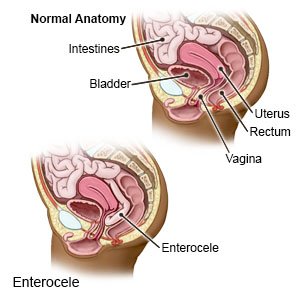
Enterocele repair
is surgery to stop part of your intestine from bulging into your vagina.
 |
How to prepare for surgery:
- Your surgeon will tell you how to prepare. You may need to arrange to take several weeks off from work. You will not be able to lift anything heavy, drive, or be physically active for several weeks after surgery. Arrange to have someone drive you home when you are discharged. You may also need to arrange for help around the house or with childcare.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about all your allergies, including medicines and anesthesia.
- Your surgeon may tell you to shower the night before your surgery. You may need to use a certain soap to help prevent a surgical site infection.
- You may be told not to eat or drink anything after midnight on the day of surgery.
What will happen during surgery:
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Surgery is usually done through the vagina. It may instead be done through small incisions in your abdomen.
- An incision will be made in the back wall of your vagina and continue over the bulging area. Your surgeon will remove the vaginal skin covering this area. Your surgeon will move the intestine back into place. The vaginal skin will be closed and tightened to repair the stretched or torn area. Connective tissues will be tightened. Your surgeon may support the repaired area by attaching it to a muscle or ligament in your pelvis. Mesh or a graft may be used if your tissues are not strong enough to hold the repair.
- The incisions will be closed. Gauze will be put into your vagina to help control bleeding. It may stay in place until the day after surgery.
What to expect after surgery:
- Medicines may be given to prevent or treat pain or a bacterial infection.
- You will need to wear sanitary pads for vaginal bleeding that occurs after surgery.
- You will be helped to walk as soon as possible after surgery. This will help to prevent blood clots in your legs.
Risks of enterocele repair surgery:
You may bleed more than expected or develop an infection. Nerve, blood vessel, bowel, or uterus damage may happen. Your bladder or urethra may be damaged. You may have trouble urinating. Even with surgery, you may develop another enterocele or other pelvic organ prolapse. Mesh may damage tissues in your vagina, or cause bleeding and discharge. Surgery may not relieve pain in your vagina, back, or hips caused by the enterocele. You may continue to have pain during sex. A fistula (abnormal opening between the vagina and rectum) may form. You may also develop a life-threatening blood clot.
Call your local emergency number (911 in the US) if:
- You have sudden chest pain or trouble breathing.
- You cough up blood.
Seek care immediately if:
- You cannot urinate.
- You soak a sanitary pad with blood every hour for 4 hours.
- You have vaginal pain that does not go away even after you take pain medicine.
- You have pus or a foul-smelling discharge from your vagina.
- You see blood in your urine.
- Your leg feels warm, tender, and painful. It may look swollen and red.
Call your gynecologist or surgeon if:
- You feel something is bulging out into your vagina or rectum and not going back in.
- You have a fever, chills, a cough, or feel weak and achy.
- You have nausea and are vomiting.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics prevent or treat a bacterial infection.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Stool softeners help make it easier for you to have a bowel movement. Some of these medicines are available without a prescription. Your healthcare provider can recommend one that might be right for you.
Self-care:
Your healthcare provider will give you specific instructions to follow. Your provider will tell you when it is okay to do certain activities. The following are general guidelines to follow in addition to instructions from your provider:
- Rest as much as possible. It is important to rest and give the surgery area time to heal. Ask when you can start doing your regular activities. This includes driving, doing housework or yard work, and going back to your job.
- Do not have sex or put anything in your vagina. The surgery area needs time to heal completely. Change your sanitary pad regularly. Keep track of how often you change the pad.
- Do not go swimming or sit in a hot tub or bath. This can lead to an infection.
- Do not lift anything heavier than 10 pounds for at least 6 weeks. Heavy lifting puts pressure on the surgery area and slows healing.
- Avoid heavy exercise. Your provider will give you an activity plan. You may need to start with light activity, such as short walks. This may be recommended 3 to 4 weeks after surgery. Your plan may increase activity as the surgery area heals.
- Do not strain when you have a bowel movement. The strain may damage the surgery area. Your bowel movements may not be regular again for a few weeks after surgery. Some pain medicines you might be taking can also cause constipation. The following can help prevent or relieve constipation:
- Drink extra liquids to help soften and move your bowels. Ask how much liquid to drink each day and which liquids are best for you.
- Eat high-fiber foods. Fiber helps move waste through your intestines. High-fiber foods include fruits, vegetables, whole-grain breads and cereals, and beans.

- Physical activity included in your activity plan will also help your bowels work better.
Follow up with your gynecologist or surgeon as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
