Complications of Infection
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What are complications of infection?
Complications can happen if an infection is not diagnosed and treated early. Some infections may have complications even when they are treated early. The infection can spread from one place in your body to the entire body through your bloodstream. Early diagnosis and treatment may prevent complications such as bacteremia, sepsis, and septic shock. These are serious, life-threatening conditions that need immediate treatment.
What types of complications can happen?
- Bacteremia is bacteria in the blood. Bacteremia can happen when infections in other parts of the body, such as the lungs, kidneys, or skin, travel to the blood. It can also happen when indwelling catheters, such as a central venous access devices, pacemaker wires, or urinary catheters become infected.
- Sepsis happens when an infection spreads and causes the body to react strongly to the germs. The body's defense system normally releases chemicals to fight off infection at the infected area. In sepsis, chemicals are released throughout the body. The chemicals cause inflammation and can cause clotting in small blood vessels that is difficult to control. Inflammation and clotting decrease blood flow and oxygen to organs. This may cause them to stop working correctly.
- Septic shock is a severe type of sepsis that happens as sepsis gets worse and causes multiple organs to shut down. The blood pressure drops very low and organs do not get enough blood. This may cause permanent damage to organs.
What increases my risk for complications of infection?
- Treatment in a hospital for a serious illness or having an indwelling catheter
- Being very young or very old
- A chronic condition, such as COPD, heart failure, or diabetes
- A weak immune system from a long-term condition or medicine
- A recent surgery or dental procedure
- Severe injuries, such as large burns
What are the signs and symptoms that an infection has become worse?
- Fever or very low body temperature with chills and violent shaking
- Swelling in the ankles or legs
- A change in mental status such as confusion, loss of consciousness, or seizures
- A fast or irregular heartbeat
- Urinating very little or not at all
- Difficulty breathing, dizziness, or weakness
- A rash or warm, red skin
How are complications of infection diagnosed?
- Measurement of your vital signs may show an abnormal temperature, heart rate, or blood pressure.
- Blood and urine tests will show infection and its cause, organ function, and information about your overall health.
- Blood gases will show how much oxygen and carbon dioxide is in the blood. The results will tell healthcare providers how well your lungs, heart, and kidneys are working.
- An x-ray, ultrasound, CT, or MRI may show the source of infection. You may be given contrast liquid to help the infection show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An EKG is a test that records your heart rhythm and how fast your heart beats. It is used to check for abnormal heart rhythms and damage to the heart from infection.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your heart. The test may show if the infection has spread to the heart valves.
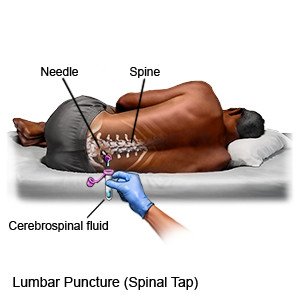
- A lumbar puncture (spinal tap) may be done to test your cerebrospinal fluid (CSF) for germs or signs of infection in or around your brain. CSF is the fluid that surrounds your spinal column and your brain.
How are complications of infection treated?
You may need any of the following, depending on how severe the complications are:
- Removal or change of a catheter may be needed to get rid of the infection.
- Medicines may be given to increase your blood pressure and blood flow to your organs. Antibiotics may be given to treat an infection. Medicines may also be given to decrease inflammation, control your blood sugar, prevent stomach ulcers, and prevent blood clots.
- Surgery or other procedures may be needed to treat problems causing sepsis or related to the complications of your infection. This may include draining an abscess or removing infected tissue.
What can I do to prevent an infection?
The following can help prevent an infection, or keep an infection from getting worse:
- Wash your hands often. Wash your hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Use soap and water every time. Rub your soapy hands together, lacing your fingers. Wash the front and back of your hands, and in between your fingers. Use the fingers of one hand to scrub under the fingernails of the other hand. Wash for at least 20 seconds. Rinse with warm, running water for several seconds. Then dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Do not touch your eyes, nose, or mouth without washing your hands first.

- Cover a sneeze or cough. Use a tissue that covers your mouth and nose. Throw the tissue away in a trash can right away. Use the bend of your arm if a tissue is not available. Wash your hands well with soap and water or use a hand sanitizer.
- Clean surfaces often. Clean doorknobs, countertops, cell phones, and other surfaces that are touched often. Use a disinfecting wipe, a single-use sponge, or a cloth you can wash and reuse. Use disinfecting cleaners if you do not have wipes. You can create a disinfecting cleaner by mixing 1 part bleach with 10 parts water.
- Ask about vaccines you may need. Vaccines help prevent infection from some viruses and bacteria. Get the influenza (flu) vaccine as soon as recommended each year, usually in September or October. Get the pneumonia vaccine if recommended. This vaccine is usually recommended every 5 years. Your provider will tell you when to get this vaccine, if needed. Get a COVID-19 vaccine and a booster as recommended. Your healthcare provider can tell you if you also need other vaccines, and when to get them.
 |
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have a seizure or lose consciousness.
- You have trouble breathing.
- Your lips or fingernails are blue.
- You feel extremely weak and have a hard time moving.
When should I seek immediate care?
- Your symptoms, such as fever, get worse, even if you are taking medicine to treat the infection.
- You have increased swelling in your legs, feet, or abdomen.
- You feel weak, dizzy, or faint.
- You stop urinating or urinate very little.
When should I call my doctor?
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
