Cold Knife Cone Biopsy
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
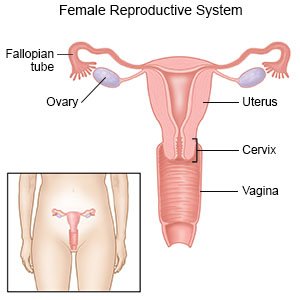
A cold knife cone biopsy
is a procedure to diagnose or treat a lesion on the cervix that may be cancer. A piece of tissue shaped like a cone is removed from the cervix.
 |
How to prepare for a cold knife cone biopsy:
- Your healthcare provider will tell you how to prepare. He or she may tell you not to eat or drink anything after midnight before the procedure. Arrange to have someone drive you home from the procedure.
- Tell your provider if you know or think you are pregnant. A pregnancy test may be done before the procedure. Your provider will tell you if you should have the biopsy during or after your pregnancy.
- Tell your provider about all your current medicines. He or she will tell you if you need to stop any medicine for the procedure, and when to stop. He or she will tell you which medicines to take or not take on the day of the procedure.
- Your provider may want to do the procedure right after your menstrual cycle ends. This helps avoid confusion with bleeding after the procedure.
- Do not have sex or put anything into your vagina for 24 hours before the procedure, or as directed.
What will happen during a cold knife cone biopsy:
- You may be given regional anesthesia to numb the procedure area. With regional anesthesia, you may feel pushing or pressure, but you should not feel pain. General anesthesia may instead be used to keep you asleep and free from pain. Your healthcare provider will apply a solution to your cervix that will help him or her find the lesion. Absorbable stitches may be used to keep the cervix in a certain position. These stitches also help lessen bleeding after the procedure.
- Your provider will use tools to remove the lesion and some tissue around it. He or she may also scrape cells off the cervix. The cells are tested for cancer.
- Any bleeding will be stopped. If stitches are used, your provider may also put packing into the area.
What to expect after a cold knife cone biopsy:
- You may have pain or cramping for a couple of weeks. You may also have bleeding or discharge from your vagina.
- Medicines may be given to prevent or treat pain or a bacterial infection.
- Packing used during the procedure will pass out of your vagina within a couple of weeks.
- Your healthcare provider will tell you how you can get the results of the biopsy. If results show you have cervical cancer, or precancer, your provider will help you make decisions about how to treat it. Treatment may include radiation, chemotherapy, targeted therapy, or surgery.
Risks of a cold knife cone biopsy:
You may have heavy bleeding during the procedure, or up to 4 weeks after. You may develop a bacterial infection. Your cervix may become too narrow. You may need a procedure to widen it if this happens. The cervix may not stay closed if you become pregnant later. You have a higher risk for preterm delivery if this happens. The risk is highest if your provider had to go deeply into your cervix to get the sample.
Call your local emergency number (911 in the US) if:
- You have sudden shortness of breath or pain when you take a breath.
- You cough up blood.
Seek care immediately if:
- You have severe pain in your lower abdomen.
- You soak through 1 sanitary pad in 1 hour or less.
- You feel weak, dizzy, or faint.
- Your leg feels warm, tender, and painful. It may look swollen and red.
Call your doctor or gynecologist if:
- You have a fever, chills, or foul-smelling discharge.
- You have bleeding with clots.
- Your bleeding is heavier than your menstrual period.
- Your pain gets worse or does not get better after you take pain medicine.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics help prevent or treat a bacterial infection.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Rest for 48 hours or as directed. Do not exercise, play sports, or lift anything heavier than 5 pounds. Ask your healthcare provider when you can return to your usual activities.
- Ask when it is okay to bathe after your procedure. Do not take a bath, swim, or soak in a hot tub until your provider says it is okay. These may increase your risk for an infection.
- Prevent a vaginal infection. Do not put anything in your vagina for 2 weeks. Do not douche, use medicines in your vagina, or have sex. These activities may cause bleeding that can lead to more stitches or a hysterectomy. Use sanitary pads instead of tampons for bleeding. Wash your hands before you clean your vagina. Do not get soap inside your vagina. Clean the area around your vaginal opening as directed.

Prevent cervical cancer:
If the biopsy shows you do not have cervical cancer, the following can help you prevent it:
- Practice safe sex. Safe sex can help decrease your risk for sexually transmitted infections (STIs) and human papillomavirus (HPV). Limit your number of sex partners. Use condoms and barrier methods for all types of sexual contact. This includes oral, vaginal, and anal sex. Use a new condom or latex barrier each time you have sex. This includes oral, vaginal, and anal sex. Make sure that the condom fits and is put on correctly.
- Ask about the HPV vaccine. The vaccine can help protect against HPV infection. It is most effective if given before sexual activity begins. This allows the body to build almost complete protection against HPV before contact with the virus. The vaccine is usually given at 11 or 12 years of age but may be given as early as 9 years. The vaccine can be given through age 26.
- Get Pap smears as directed. The Pap smear can help diagnose cervical cancer in an early stage. Cancer that is in an early stage may be easier to treat. Pap smears usually start at age 21 and continue until age 65. A Pap smear alone may be done every 3 years. An HPV test alone or with a Pap smear may be done every 5 years, starting at age 30. Your healthcare provider will tell you if you need to have Pap smears more often or after age 65.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can increase your risk for cervical cancer. Ask your healthcare provider for more information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Follow up with your doctor or gynecologist as directed:
You may need to go in to get your biopsy results. Write down your questions so you remember to ask them during your visits.
For support and more information:
- American Cancer Society
250 Williams Street
Atlanta , GA 30303
Phone: 1- 800 - 227-2345
Web Address: http://www.cancer.org
- National Cancer Institute
6116 Executive Boulevard, Suite 300
Bethesda , MD 20892-8322
Phone: 1- 800 - 422-6237
Web Address: http://www.cancer.gov
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
