Chronic Liver Disease
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is chronic liver disease (CLD)?
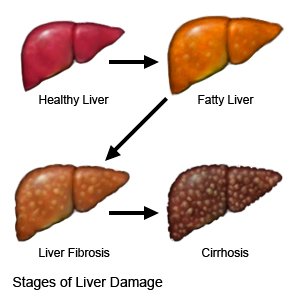
CLD is the gradual worsening of the liver for more than 6 months. The liver makes enzymes and bile that help digest food and gives your body energy. It also removes harmful material from your body, such as alcohol and other chemicals. Repeated swelling and damage to your liver over time causes scar tissue to form. Scar tissue starts to replace healthy liver tissue. The scar tissue prevents the liver from working properly.
 |
What increases my risk for CLD?
- Long-term alcohol use
- Hepatitis B or C infection
- Fat or iron buildup in the liver
- A disease such as type 2 diabetes, cystic fibrosis, or a family history of liver cancer
- Long-term use of certain medicines, such as acetaminophen or anabolic steroids
- Damage to the bile ducts that blocks the flow of bile
- Obesity or certain autoimmune conditions
What are the signs and symptoms of CLD?
You may not have any signs or symptoms until your liver damage is severe. You may have any of the following:
- Fatigue (being mentally and physically tired), confusion
- Bleeding and bruising easily
- Swelling of your feet, legs, or abdomen
- Vomit that looks like it has coffee grinds or blood in it
- Itchy skin or jaundice (yellowing of your skin or the whites of your eyes)
- Pain or discomfort in the upper right part of your abdomen
- Black bowel movements or dark urine
How is CLD diagnosed?
- Blood tests may be used to check your liver enzymes. This test shows how well your liver is working.
- An ultrasound may show the size and structure of your liver. It may also show damage to your liver or other tissues or organs.
- CT or MRI pictures may be taken of your liver. You may be given contrast liquid to help your liver show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. The MRI machine uses a powerful magnet. Do not enter the MRI room with anything made of metal. Metal can cause serious injury from the magnet. Tell the healthcare provider if you have any metal in or on your body.
- A liver biopsy is a procedure used to take a small piece of your liver to be tested for damage.
How is CLD treated?
Treatment depends on the cause of your liver disease. The following may be used:
- Medicines may be used to treat high blood pressure in the portal vein (the blood vessel that goes to your liver). You may also need medicine to decrease extra fluid that collects in an area such as your legs or abdomen. Medicines may be used to decrease itching, or to treat a bacterial or viral infection.
- An endoscopy may show swollen veins in the esophagus or stomach. An endoscope is a bendable tube with a light and camera on the end. It is placed through the mouth and down the throat.
- Surgery may be used to create a channel inside your liver to increase blood flow. This will help decrease swelling in your abdomen and lower blood pressure in the portal vein. Your risk for bleeding in your esophagus and stomach will also be decreased. You may need a liver transplant if your liver fails (stops working).
What can I do to manage or prevent CLD?
- Do not drink alcohol. Alcohol will cause more damage to your liver. Ask your healthcare provider for information if you currently drink alcohol and need help to quit.
- Monitor your weight. You may need to weigh yourself daily and keep a record. This will help providers monitor any buildup of fluid in your body.
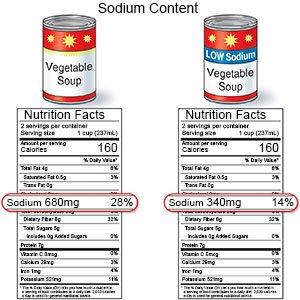
- Limit sodium (salt). You may need to decrease the amount of sodium you eat if you have swelling caused by fluid buildup. Sodium is found in table salt and salty foods such as canned foods, frozen foods, and potato chips.
- Drink liquids as directed. You may need to drink less liquid than usual. Ask how much liquid to drink each day and which liquids are best for you.
- Ask about vaccines. Your body may have a hard time fighting infection due to CLD. Vaccines help protect you against viruses that can cause diseases such as the flu or hepatitis. Viral hepatitis is caused by a virus that leads to inflammation of the liver. You may need a hepatitis A or B vaccine. No vaccine is available for hepatitis C. Your provider can give you information on how to prevent a hepatitis C infection. You may also need a pneumonia vaccine. Always get a flu vaccine as soon as recommended each year, usually in September or October.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage and make CLD harder to manage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes and smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Ask about medicines. Some medicines can harm your liver. Avoid NSAIDs such as ibuprofen, naproxen, or similar medicines. Talk to your provider about all your medicines. Do not take any over-the-counter medicine or herbal supplements unless your provider says it is okay.
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meat, and fish. Ask if you need to be on a special diet.

Call your local emergency number (911 in the US) or have someone call if:
- You have a seizure.
- You have chest pain.
- You lose consciousness or cannot be woken.
- You have sudden shortness of breath or trouble breathing.
When should I seek immediate care?
- You have pain during a bowel movement and it is black or contains blood.
- You have a fast heart rate and fast breathing.
- You are dizzy or confused.
- You have severe pain in your abdomen.
- Your vomit looks like it has coffee grinds or blood in it.
When should I call my doctor?
- Your abdomen or legs start to swell.
- You have a fever.
- You have red or itchy skin.
- You are in pain and feel weak.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
