Carotid Endarterectomy
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
What you need to know about carotid endarterectomy (CEA):
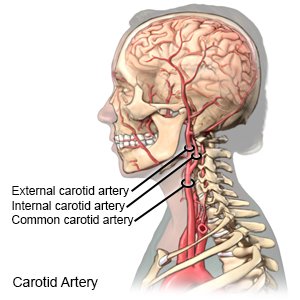
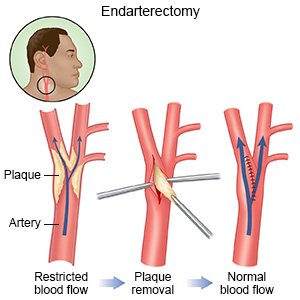
CEA is surgery to remove plaque (fatty deposits) from inside your carotid artery. The carotid artery is a blood vessel found on both sides of your neck. Plaque may build up inside your carotid artery and decrease blood flow to your brain. A piece of plaque may also break free and cause a stroke.
 |
How to prepare for surgery:
- Your surgeon will tell you how to prepare. You may be told not to eat or drink anything after midnight on the day of surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. Your surgeon will tell you if you need to take aspirin or a blood-thinning medicine before surgery. This medicine will help stop clots from forming in your blood. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- You may need blood tests before surgery. You may also need an ultrasound, CT scan, or MRI. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the provider if you have any metal in or on your body. The tests may be done to check the plaques in your carotid artery. Angiography may be used to check the blood flow from your carotid artery to your brain.
- You may need tests to make sure your heart is healthy enough for surgery. This may be needed if you have heart failure or are at increased risk for a heart attack.
What will happen during surgery:
- You will be given regional or general anesthesia to prevent pain during surgery. An incision will be made in your neck, over your carotid artery. Your surgeon will make an incision in the artery. The plaque will be separated from the artery wall and removed.
- The artery will be closed or put back together with stitches. An artificial patch or a piece of your own vein may also be used to close your artery. The blood flow through your carotid artery will be checked.
- A drain may be used to remove extra blood and fluid from around your artery. Your skin will be closed with stitches and covered with a bandage.
 |
What to expect after surgery:
Healthcare providers will remove the bandage soon after surgery to check the incision. Do not get out of bed until your healthcare provider says it is okay.
- Your head will be kept straight for 24 hours after surgery. This helps lower your risk for side effects, such as swelling and fainting. The head of your bed may also be slightly raised.
- Medicines may be given to thin your blood to prevent blood clots. You may also need medicine to lower your cholesterol or blood pressure level.
- Ultrasound pictures may be used to look for clots in your carotid artery.
Risks of CEA:
- Muscles or nerves near your carotid artery may be damaged. Nerve damage may lead to changes in how you look, or trouble chewing and swallowing. You may bleed more than expected or develop an infection. You may have headaches, high blood pressure, or abnormal heartbeats. Swelling in your surgery area may block your airway. A fistula (abnormal connection) may form between your carotid artery and another tissue. You are also at risk for a life-threatening heart attack during or after surgery.
- You may get a blood clot in your leg, arm, or carotid artery. The clot may travel to your heart or brain and cause life-threatening problems, such as a heart attack or stroke. After CEA, your carotid artery may become narrow or full of plaque again. The patch used for your surgery may tear or loosen, causing a large amount of blood loss.
Call your local emergency number (911 in the US) for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You suddenly feel lightheaded and short of breath.
- You have chest pain when you take a deep breath or cough.
- You cough up blood.
Drugs used to treat this and similar conditions
Crestor
Crestor (rosuvastatin) is used to treat high cholesterol and high triglycerides in the blood ...
Plavix
Plavix (clopidogrel) is used to prevent blood clots after a recent heart attack or stroke. Includes ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Xarelto
Xarelto (rivaroxaban) is a factor Xa inhibitor used to reduce the risk of blood clots and stroke in ...
Zontivity
Zontivity is used for the prevention of cardiovascular events. Includes Zontivity side effects ...
Vorapaxar
Vorapaxar systemic is used for peripheral arterial disease, prevention of atherothrombotic events ...
Rivaroxaban
Rivaroxaban systemic is used for atrial fibrillation, cardiovascular risk reduction, congenital ...
Rosuvastatin
Rosuvastatin is a prescription medication used to treat high cholesterol and prevent heart disease ...
Clopidogrel
Clopidogrel systemic is used for acute coronary syndrome, acute coronary syndrome, prophylaxis ...
Isoxsuprine
Isoxsuprine systemic is used for cerebrovascular insufficiency, coronary artery disease, raynaud's ...
Seek care immediately if:
- Your incision is swollen, red, or has pus coming from it.
- Blood soaks through your bandage.
- Your stitches come apart.
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
Call your doctor or vascular surgeon if:
- You have nausea or are vomiting.
- You have a fever or chills.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Aspirin helps thin the blood to keep blood clots from forming. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead. Do not take more or less aspirin than directed. This medicine makes it more likely for you to bleed or bruise.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Blood pressure medicine helps keep your blood pressure under control. This will protect your surgery site from breaking open.
- Cholesterol medicine helps lower the amount of cholesterol in your blood. It may help decrease new plaque from forming in your carotid artery.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Warning signs of a stroke:
The word F.A.S.T. can help you remember and recognize warning signs of a stroke.
- F = Face: One side of the face droops.
- A = Arms: One arm starts to drop when both arms are raised.
- S = Speech: Speech is slurred or sounds different than usual.
- T = Time: A person who is having a stroke needs to be seen immediately. A stroke is a medical emergency that needs immediate treatment. Some medicines and treatments work best if given within a few hours of a stroke.
Self-care:
- Carefully wash the surgery area with soap and water. Dry the area and put on new, clean bandages as directed. Change your bandages if they get wet or dirty.
- Do not lift anything heavy until your healthcare provider says it is okay. This may be for a few weeks after surgery.
- Ask when you can return to your regular daily activities. Your provider will tell you when you can go back to work, drive, or do other activities.
Manage or prevent carotid artery or heart disease:
- Manage any other health conditions. Health conditions such as diabetes or high blood pressure or cholesterol levels can increase your risk. Your healthcare providers can help you manage any health conditions you have.
- Eat a variety of healthy foods. Healthy foods include fruit, vegetables, whole-grain breads, low-fat dairy products, lean meat, and fish. Choose fish that are high in omega-3 fatty acids, such as salmon and fresh tuna. Ask your provider for more information on a heart healthy diet and the DASH eating plan.

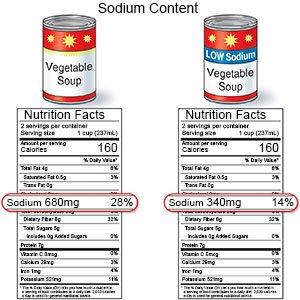
- Limit sodium (salt). Sodium may increase your blood pressure. Add less table salt to your foods. Read food labels and choose foods that are low in sodium. Your provider may suggest you follow a low-sodium diet.
- Reach or maintain a healthy weight. Extra weight makes your heart work harder. Ask your provider what a healthy weight is for you. Your provider can help you create a safe weight loss plan, if needed.
- Exercise as directed. Exercise helps improve heart function and can help you manage your weight. Exercise can also help lower your cholesterol and blood sugar levels. Try to be active every day. Your provider can help you create an exercise plan that works best for you.
- Limit alcohol. Alcohol can increase your blood pressure and triglyceride levels. Men should limit alcohol to 2 drinks per day. Women should limit alcohol to 1 drink per day. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart and lung damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
Follow up with your doctor or vascular surgeon as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
