Cardioversion
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
What you need to know about cardioversion:
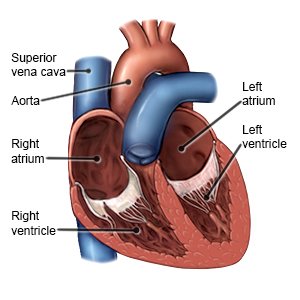
Cardioversion is a procedure that uses medicine or electrical shocks to correct arrhythmias. An arrhythmias is a heartbeat that is too slow, too fast, or irregular. It may prevent your body from getting the blood and oxygen it needs. Your heart has 4 chambers, called the atria and ventricles. The atria are at the top of your heart, and the ventricles are at the bottom of your heart. Most arrhythmias that need cardioversion start in the atria.
 |
How to prepare for cardioversion:
You may need a transesophageal echocardiogram (TEE) before your cardioversion. A TEE is an ultrasound to check for clots in your heart. You may need to take blood thinner medicine for several weeks before your cardioversion. This will help prevent blood clots. Your provider will talk to you about how to prepare for cardioversion. He or she may tell you not to eat or drink anything after midnight on the day of your cardioversion. He or she will tell you what medicines to take or not take on the day of your cardioversion. Arrange for someone to drive you home and stay with you for 24 hours. This person can call 911 if you have problems after your cardioversion.
What will happen during a chemical cardioversion:
You will be placed on a heart monitor. A heart monitor is an EKG that records your heart's electrical activity. Your provider will inject 1 or more medicines into your IV. The medicines will help change your heartbeat to a normal rhythm. You may feel light headed, dizzy, or nauseous. You may have pain or pressure in your chest, jaw, shoulders, or arms. These symptoms are normal, and usually last for a minute or less. You may need electrical cardioversion if chemical cardioversion does not change your heartbeat to a normal rhythm.
What will happen during an electrical cardioversion:
You will be given medicine through your IV to keep you asleep and free from pain. You will be placed on a heart monitor. A heart monitor is an EKG that records your heart's electrical activity. A provider will also monitor your blood pressure and oxygen levels during the procedure. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils.
- In external cardioversion your provider will place sticky pads on your chest and back. Your heart will be shocked with electricity through the pads. Your heart may be shocked more than once to help it return to its normal rhythm.
- In internal cardioversion your provider will insert a catheter through a vein and into your heart. Your heart will be shocked through the catheter. Your heart may be shocked more than once to help it return to its normal rhythm.
What will happen after cardioversion:
Providers will monitor your heartbeat, blood pressure, and oxygen levels. You may feel drowsy from the medicine you were given during the procedure. Your chest may be red or sore where the pads were placed. This should go away in a few days. You may go home when they say it is okay or you may need to stay in the hospital.
Risks of cardioversion:
Your skin may be burned from the electrical shocks. Cardioversion may cause a blood clot to travel to your heart or brain and cause a heart attack or stroke. You may develop a life-threatening arrhythmia or low blood pressure during cardioversion. You may need medicine or more electric shocks to treat this. Even with cardioversion, your heartbeat may not change or may not stay regular.
Drugs used to treat this and similar conditions
Isuprel
Isuprel is used for adams-stokes syndrome, AV Heart Block, bronchospasm during anesthesia, cardiac ...
Adrenalin
Adrenalin is used for adams-stokes syndrome, allergic reactions, anaphylaxis, asthma, acute ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Betapace
Betapace and Betapace AF tablets are antiarrhythmic drugs used in the treatment of ventricular ...
Tikosyn
Tikosyn (dofetilide) is antiarrhythmic drug used to treat an abnormal heartbeat including atrial ...
Epsom Salt
Epsom Salt is used for barium poisoning, hypomagnesemia, seizure prevention, ventricular arrhythmia
Verapamil
Verapamil is used to treat hypertension (high blood pressure), angina (chest pain), and certain ...
Calcium chloride
Calcium chloride systemic is used for asystole, electromechanical dissociation, hyperkalemia ...
Propranolol
Propranolol is a beta-blocker that is used to treat tremors, chest pain, high blood pressure, heart ...
Call 911 for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You have trouble breathing.
Seek care immediately if:
- You feel your heart beating fast or fluttering.
- You feel weak or faint.
- Your leg or arm is larger than usual, painful, and warm.
Contact your healthcare provider if:
- Your skin is itchy, swollen, or you have a rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Heart medicines help control your heart rate and rhythm.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Rest as directed. Do not drive for at least 24 hours. Ask your provider when you can return to your normal activities.
- Check your heart rate and blood pressure as directed. Ask your provider what your heart rate and blood pressure should be.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart and lung damage. They can also increase your risk for another arrhythmia. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Eat heart healthy foods. These include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil.
- Maintain a healthy weight. Ask your provider how much you should weigh. Ask him or her to help you create a weight loss plan if you are overweight.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
