Cancer Pain
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What do I need to know about cancer pain?
Pain may be caused by cancer, treatment for cancer, or a procedure to diagnose cancer. A tumor or another condition caused by cancer may also cause pain. Your pain may get better after you finish treatment or if your cancer is in remission. Proper control of pain that continues can help improve your quality of life.
How is the cause of cancer pain diagnosed?
Your healthcare provider will examine you and ask where your pain is, what it feels like, and when it started. Tell your provider if your pain comes and goes or is constant. Tell your provider if anything helps your pain or makes it worse. You may need any of the following:
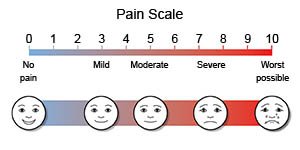
- Pain scales use numbers or faces to help you describe how bad your pain is. Your provider may ask you to rate your pain on a scale from 0 to 10.
- An x-ray, CT, or MRI may show the cause of your pain. You may be given contrast liquid to help the area show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Stimulation tests may help to find which nerves or muscles are affected by pain. These tests may include nerve conduction or muscle function studies.
How is cancer pain treated?
Treatment depends on the cause, type, and severity of your pain. Talk to your healthcare provider about pain control before, during, and after certain tests, procedures, or treatments. You may need any of the following:
- Medicines
- Acetaminophen or NSAIDs , such as ibuprofen, may help decrease pain and inflammation. Talk to your provider before you take these medicines if you are getting chemotherapy (chemo). Acetaminophen increases the risk for liver damage and NSAIDs increase the risk for kidney damage. Chemo can increase the risk for these problems even more. Your provider may recommend you wait to use these medicines until after you complete chemo.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Local anesthetics can be rubbed on your skin or injected into a nerve or muscle to numb an area.
- Other medicines may be given to decrease pain, inflammation, or muscle spasms.
- Procedures may be done to block nerve or pain signals.
- Surgery may be needed if other treatments do not work.
How else may cancer pain be treated?
- Cognitive behavior therapy (CBT) teaches you ways to cope with your pain.
- Acupuncture uses very thin needles to balance energy channels in the body. This is thought to help reduce pain and other symptoms.
- Massage therapy or acupressure may help relax tight muscles and decrease pain.
- A transcutaneous electrical nerve stimulation (TENS) unit uses mild, safe electrical signals to help control pain. The device is placed over the area of pain and attaches to your skin.
- Radiation therapy may be used to decrease bone pain.
What do I need to know about prescription pain medicine safety?
- Take your medicine as directed. Take only the amount prescribed or recommended by your provider. Do not take more medicine if you have breakthrough pain. Too much medicine may cause breathing problems or other health issues. Tell your provider if your medicine does not control your pain.
- Do not mix prescription pain medicines. This can cause an overdose of medicine, which can become life-threatening. Read the medicine labels. Make sure you know the ingredients in all your medicines.
- Store prescription pain medicine in a safe place at home. Keep your medicine away from children and other people. Never share your medicine with anyone.
What can I do to help manage my pain?
- Apply heat or ice to the area. Heat helps decrease muscle spasms. Ice helps decrease inflammation. Your healthcare provider may recommend only heat or ice, or you may be told to alternate. For heat, use a heat pack, heating pad, or a warm washcloth. Apply heat for 20 to 30 minutes every 2 hours for as many days as directed. For ice, use an ice pack, or put crushed ice in a plastic bag. Cover the ice pack with a towel before you place it on your skin. Apply ice for 15 to 20 minutes every hour or as directed.
- Be physically active, as directed. Physical activity such as exercise can help decrease pain and improve your body function. Ask your healthcare provider about the best exercise plan for you.
- Practice mindfulness or relaxation techniques. Yoga, meditation, or deep breathing can help you relax and distract you from thinking about your pain.
- Join a support group. It may be helpful for you to talk with others who have similar conditions. Tell your healthcare provider, family, or friends about your feelings. Your provider can give you resources to help you cope.
Call your local emergency number (911 in the US) or have someone call if:
- You are breathing slower than usual, or you have trouble breathing.
- You have trouble staying awake, or you lose consciousness.
- You take too much pain medicine by mistake.
- You have a seizure.
When should I seek immediate care?
- You have a fever.
- Your pain gets worse, even after you take medicine.
- You have new symptoms, such as numbness or tingling.
When should I call my doctor?
- You have side effects from your pain medicine, such as itching, nausea, or vomiting.
- Your pain causes trouble sleeping.
- You do not think your medicine is working.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
