CABG (Coronary Artery Bypass Graft)
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
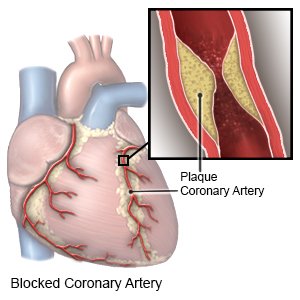
A coronary artery bypass graft (CABG) is open heart surgery to clear blocked arteries in your heart. CABG surgery improves blood flow to your heart by bypassing (sending blood around) the blocked part of an artery. This restores blood flow to your heart and helps prevent a heart attack.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) or have someone call if:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You have a fast heartbeat that flutters.
- You feel like you are going to faint.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have numbness or tingling in your arms or legs.
- You have a severe headache.
- You have a fever higher than 101°F (38.4°C).
Call your doctor if:
- You have gained 2 pounds in 24 hours.
- Your wound is red, swollen, or draining pus.
- You feel depressed.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Cholesterol medicine helps lower cholesterol and lipid levels in your blood.
- Antibiotics help prevent a bacterial infection.
- Heart medicine helps strengthen and regulate your heartbeat.
- Blood pressure medicine helps lower or control your blood pressure.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Drugs used to treat this and similar conditions
Crestor
Crestor (rosuvastatin) is used to treat high cholesterol and high triglycerides in the blood ...
Ranexa
Ranexa (ranolazine) is used to chronic treat angina (chest pain). Learn about side effects ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Ibuprofen
Ibuprofen (Advil, Motrin) treats minor aches and pains caused by the common cold, headaches ...
Gabapentin
Gabapentin is an anti-epileptic drug, also called an anticonvulsant. It is used to treat some types ...
Nitroglycerin
Nitroglycerin systemic is used for anal fissure and fistula, angina, angina pectoris prophylaxis ...
Tramadol
Tramadol is an opioid medication that may be used to treat moderate to moderately severe chronic ...
Tylenol
Tylenol is a pain reliever and a fever reducer used to treat many conditions such as headaches ...
Acetaminophen
Acetaminophen is a widely used pain reliever and fever reducer for conditions like headaches ...
Go to cardiac rehabilitation (rehab) as directed:
Cardiac rehab is a program run by specialists who will help you safely strengthen your heart and prevent more heart disease. This plan includes exercise, relaxation, stress management, and heart-healthy nutrition. Healthcare providers will also check to make sure any medicines you take are working. The plan may also include instructions for when you can drive, return to work, and do other normal daily activities.
Care for your surgery area as directed:
Carefully wash around the area with soap and water. Let the soap and water run over the area. Do not scrub the area. If you do not have a bandage, gently pat the area dry with a clean towel. If you have a bandage, dry the area and put on a new, clean bandage. Change your bandage if it gets wet or dirty.
Activity:
Your healthcare provider will give you specific activity instructions. The following are general guidelines to follow for up to 8 weeks after surgery:
- Protect your sternum. Hug a pillow to your chest or cross your arms over your chest when you laugh, sneeze, or cough.
- Be careful when you get into or out of a chair or bed. Hug a pillow or cross your arms when you stand or sit. Do not twist as you move. Use only your legs to sit and stand. You may need to use a raised toilet seat if you have trouble standing up without using your arms. Your healthcare provider may teach you to use your elbow for support as you move from lying to sitting.
- Do not lift anything heavier than 5 pounds until your healthcare provider says it is okay. For example, a gallon of milk weighs 8 pounds.
- Do not play sports that use your shoulder. Examples include tennis and golf.
- Do not drive until your healthcare provider says it is okay.
- Keep your arms down as much as possible. Do not put your arms out to the side, behind you, or over your head. Do not let anyone pull your arms to help you move or dress. Do not reach for items.
- Do not push or pull anything. Examples include a car door or a vacuum cleaner.
Prevent another blocked artery:
- Manage other health conditions. Diabetes and high cholesterol increase your risk for a heart attack and stroke. Talk to your healthcare provider about your management plan. He or she will make a plan that helps you manage your conditions.
- Eat heart-healthy foods. You may need to eat foods that are low in salt, fat, or cholesterol. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask your healthcare provider for more information about a heart healthy diet.

- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart and lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Extra weight can increase the stress on your heart. Ask him or her to help you create a safe weight loss plan if needed.
Ask about vaccines you may need:
Vaccines help prevent diseases that can be dangerous for a person who has heart disease. Ask your healthcare provider about these and other vaccines you may need:
- Get a flu vaccine as soon as recommended each year, usually starting in September or October.
- Get a pneumonia vaccine is recommended for all adults 65 or older. Your provider may also recommend this vaccine if you are younger than 65.
- Get a COVID-19 vaccine as directed. At least 1 dose of an updated vaccine is recommended for everyone 6 months or older. COVID-19 vaccines are given as a shot in 1 to 3 doses, depending on the age of the person who receives it. COVID-19 vaccines are updated throughout the year. Your healthcare provider can help you schedule all needed doses as updated vaccines become available.
Follow up with your doctor or cardiologist as directed:
You may need to go in regularly for tests to check how your heart is doing. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
