Bowel Incontinence
Medically reviewed by Drugs.com. Last updated on Jun 2, 2025.
What is bowel incontinence?
Bowel incontinence is when you lose control over your bowel movement. Liquid or solid bowel movement may leak from your anus. Bowel incontinence may be a short-term or long-term problem.
What are the types of bowel incontinence?
Bowel incontinence ranges from a small amount of leaking to losing complete control over your bowel movement. There are 3 types of bowel incontinence:
- Urge incontinence is when you feel your bowels are full, but you cannot control when the bowel movement comes out. There may be a problem with the muscles or nerves that control your bowels.
- Passive incontinence is when you have a bowel movement without knowing. Your body may not feel when your rectum is ready to pass a bowel movement.
- Seepage is when bowel movement leaks from your anus because your bowels did not empty completely.
What causes bowel incontinence?
Muscles in your pelvic floor, anus, and rectum work together to hold your bowel movement in. Nerves work with the muscles so your body knows when it is time for a bowel movement. Problems with any of these muscles or nerves can cause bowel incontinence. The following are also possible causes:
- Diarrhea may fill your rectum quickly and make it harder for the muscles of the anus and rectum to hold in. Chronic diarrhea can cause these muscles to weaken over time.
- Constipation may weaken muscles of your anus and rectum over time. Straining when you have a bowel movement may cause nerve damage. Constipation may lead to seepage. Liquid bowel movement will seep through the firm bowel movement that is stuck in your rectum.
- Muscle damage or weakness may be caused by vaginal birth or surgery to the anus or rectum. Muscles in your anus may have trouble staying closed.
- Nerve damage may happen during vaginal birth or surgery to the anus or rectum. Neurologic disorders such as multiple sclerosis, stroke, or dementia may also cause damage to your nerves. Nerve damage may reduce feeling in your rectum. You may not feel that you need to have a bowel movement.
- Scarring of the muscles or tissue near the rectum or anus may cause stiffness. This makes it hard for the rectum and anus to hold bowel movement in. Surgery, radiation treatment, and diseases that cause inflammation may cause scarring and stiffness.
- Conditions such as hemorrhoids or rectal prolapse may prevent muscles around your anus from closing properly. Small amounts of liquid bowel movement may leak out.
What increases my risk for bowel incontinence?
- Age older than 65
- Physical disability or an injury to your spinal cord
- Obesity, overweight, or lack of exercise
- Childbirth, especially a vaginal delivery
- Conditions such as ulcerative colitis or Crohn disease
- Having multiple medical conditions
- Certain medicines such as antibiotics or laxatives
What are the signs and symptoms of bowel incontinence?
- You cannot control your bowel movement.
- Your bowels do not feel empty after a bowel movement.
- Your notice bowel movement in your underwear.
- You often leak bowel movement during your daily activities.
- You leak bowel movement when you pass gas.
- You leak bowel movement when you cough, sneeze, exercise, or laugh.
How is bowel incontinence diagnosed?
Your healthcare provider will ask about your symptoms, medical history, and current medicines. You may need any of the following:
- A digital rectal exam will look for problems in your anus, rectum, and surrounding area. Your provider will put a gloved finger inside your rectum to check the strength of your anal muscles.
- A pelvic exam is used to check your internal reproductive organs by feeling their size and shape. Your provider will use a speculum to widen your vagina. You will strain or push down like you are having a bowel movement. You may be asked to tighten the muscles of your pelvis. This helps your provider check the strength of your pelvic muscles.
- Blood or urine tests may be used to check for an infection or get information about your overall health. These tests may also show if a condition is causing your bowel incontinence, such as anemia or type 2 diabetes.
- A bowel movement sample will be tested for blood or an infection.
- A bowel function test will check how well the muscles and nerves of your anus, pelvic floor, and rectum work. Types of bowel function tests include anorectal manometry, defecography, or electromyography. Your provider will tell you more about these tests.
- An endoscopy is a procedure to examine the inside of your anus, rectum, and colon (large intestine). A flexible tube with a small light and camera on the end is inserted into your rectum. A small tissue or bowel movement sample may be removed. These are sent to a lab for testing.
- X-ray, ultrasound, or MRI pictures may be used to check for problems in your anus, rectum, or colon. You may be given contrast liquid to help these areas show up better in the pictures. Tell healthcare providers if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
How is bowel incontinence treated?
Treatment depends on the cause of your bowel incontinence. You may need any of the following:
- Medicines may help treat diarrhea or constipation. Your healthcare provider may also recommend fiber supplements, such as psyllium. Fiber supplements help bulk your bowel movement and decrease bowel incontinence. Ask your provider which type of fiber is right for you.
- Devices may be used to help decrease bowel movement leakage.
- A vaginal balloon is placed and inflated inside your vagina. The balloon puts pressure on your rectum and helps keep the muscles closed.
- Sacral nerve stimulation sends electrical impulses directly to the sacral nerves to improve or restore bowel function. Sacral nerves are in your lower back. They control the anus, rectum, and bladder functions.
- Biofeedback and pelvic floor physical therapy help teach you how to do pelvic muscle exercises. A device may be used to help strengthen your pelvic muscles. Strong pelvic muscles will help you hold the bowel movement in until you reach the bathroom. It may also help you feel when your rectum is filling with bowel movement.
- Bulking agents may be injected into the wall of your anus to make it thicker. This helps to keep your anus closed and decreases bowel movement leakage.
- Surgery may treat causes of bowel incontinence such as hemorrhoids or rectal prolapse. You may also need surgery if other treatments do not work. Several types of surgery can help improve your bowel control. Ask your provider for more information about these surgeries.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage bowel incontinence?
- Relieve anal discomfort. You may have irritation, itching, or pain around your anus. Relieve discomfort by washing the area after each bowel movement. Keep the area dry and wear loose-fitting clothing. A moisture-barrier cream may reduce discomfort. Ask your healthcare provider which cream is best for you.
- Do pelvic muscle exercises as directed. Your pelvic muscles help control your bowel movement. Pelvic exercises involve tightening and relaxing pelvic muscles. Squeeze these muscles tight for 5 seconds, then relax for 5 seconds. Gradually work up to squeezing for 10 seconds. Do 3 sets of 15 repetitions a day, or as directed. These exercises can make the pelvic muscles stronger and improve bowel control.
- Keep a bowel incontinence record. Write down how often you leak bowel movement and how much you leak. Make a note of what you were doing when you leaked.
- Keep a food diary. Keep a list of food and liquids you have each day. Write down any symptoms that develop. This will help to see if a certain food causes your symptoms. Bring this to your follow-up visits.
- Prevent constipation. Eat a variety of high-fiber foods. Good examples are high-fiber cereals, beans, vegetables, and whole-grain breads. Prune juice may help make your bowel movement softer. Walking is the best way to trigger your intestines to have a bowel movement.

- Prevent diarrhea. Certain foods may loosen your bowel movement. Avoid caffeine, alcohol, fruit juice, and prunes. Do not eat beans, cabbage, or smoked or cured meat. Avoid dairy products and spicy foods.
- Drink liquids as directed. Ask your provider how much liquid to drink each day and which liquids are best for you.
- Train your bowel. A bowel program may help you learn how to plan for a bowel movement. For example, you will go to the bathroom at set times, such as every 2 hours or right after a meal. You will do this even if you do not feel the urge to go.
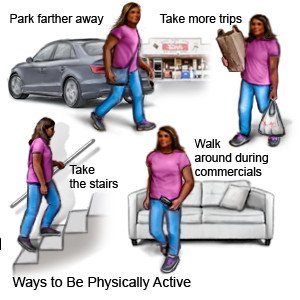
- Be physically active and maintain a healthy weight. Ask your provider what a healthy weight is for you. Extra weight puts pressure on your pelvic muscles and may make your symptoms worse. Your provider can help you create a weight loss plan, if needed. The plan will include ways to be physically active that will not put extra pressure on your pelvic muscles.
When should I seek immediate care?
- You have severe abdominal pain.
- You have blood in your bowel movement.
- You have trouble eating, drinking, or keeping food down.
- Your skin, mouth, and tongue are dry, and you feel very thirsty.
- You feel lightheaded, weak, or faint.
- You are confused or cannot think clearly.
When should I call my doctor?
- You have a fever.
- You have new symptoms.
- Your symptoms do not improve, or they get worse.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Bowel Incontinence
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
