Atelectasis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is atelectasis?
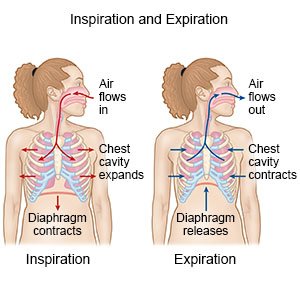
Atelectasis is a condition that happens when the alveoli in your lungs cannot expand fully. This may cause part or all of your lung to collapse. Alveoli are tiny air sacs in your lungs. Alveoli exchange oxygen and carbon dioxide and help put oxygen into your blood. The exchange of oxygen and carbon dioxide cannot take place in the alveoli when your lung collapses.
 |
What causes atelectasis?
- Bronchial blockage by mucus plugs, foreign bodies, or swelling due to lung disease
- Decreased surfactant production (surfactant keeps the alveoli in your lung from collapsing when you exhale)
- Any squeezing that does not allow your lungs to open fully, such as a tight bandage
- Any pain that prevents you from taking a deep breath, such as from a rib fracture, or a chest or abdomen incision
What increases my risk for atelectasis?
- General anesthesia
- Surgery on your chest, upper abdomen, head and neck, or blood vessels
- Not moving for long periods of time, such as while in intensive care or on bed rest
- A chronic lung disease, such as COPD or cystic fibrosis
- Obesity, smoking, or age older than 60
- A health condition such as heart failure, obstructive sleep apnea, or pulmonary hypertension
What are the signs and symptoms of atelectasis?
You may not have any symptoms, or you may have any of the following:
- Cough or wheeze
- Shortness of breath
- Chest pain
- Severe sweating
- A fast heartbeat
How is atelectasis diagnosed?
Your healthcare provider will listen to your lungs. Your provider may tap on areas of your back and chest. You may also need any of the following:
- Blood tests check for infection and measure your oxygen level.
- An x-ray, CT, or MRI may show if your lungs have collapsed. You may be given contrast liquid to help the lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An ultrasound may show if you have fluid in your lungs.
- A bronchoscopy may be done if the cause of your atelectasis is not known. A bronchoscope (thin tube with a light) is inserted into your mouth and moved down your throat to your lungs. Tissue and fluid may be collected from your airway or lungs to be tested.
How is atelectasis treated?
If your lung has collapsed, you may need to be admitted to the hospital for treatment. You also may need any of the following:
- Medicines may be given to help thin mucus so that it is easier to cough out. You may be given medicines that help open your airways or treat an infection. You may be given pain medicine if your pain prevents you from breathing deeply.
- Surgery or radiation may be done to remove or shrink a blockage in your airways.
How can I manage or prevent atelectasis?
- Change your position often. Sit on the side of the bed or walk after surgery as directed. This helps expand your lungs. Your healthcare provider may ask you to lie or sit in certain positions to help drain mucus. This is called postural drainage.
- Use chest percussion. Chest percussion is gentle clapping on your back or side to help move mucus out of your lungs. Chest percussion is sometimes used with postural drainage. Ask your provider for more information about postural drainage and chest percussion.
- Cough often. This can help clear mucus from your lungs.
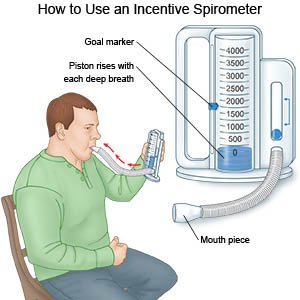
- Do deep breathing exercises. This can help improve your lung function and decrease your risk for atelectasis. An incentive spirometer may be used to help you breathe deeply and slowly. Put the plastic piece in your mouth and take a slow, deep breath. Then let the air out and cough. Repeat these steps as directed. Ask your provider for more information on deep breathing exercises.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Drink liquids as directed. Liquids help loosen mucus. Ask how much liquid to drink each day and which liquids are best for you.
Call your local emergency number (911 in the US) or have someone call if:
- You have sudden trouble breathing.
- You have severe chest pain.
- Your lips or fingers look blue.
When should I seek immediate care?
- The skin around your neck and ribs pulls in with each breath.
When should I call my doctor?
- You are coughing up a large amount of mucus.
- You are more tired than usual.
- You have trouble catching your breath while you exercise or walk up stairs.
- You have a fever.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Atelectasis
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
