ARDS (Acute Respiratory Distress Syndrome)
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
You may need to use oxygen or have other ongoing treatment after discharge. You will get specific instructions for when and how to use oxygen safely. Work with your doctor and pulmonologist to schedule follow-up visits and tests.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for any of the following:
- You have trouble breathing or shortness of breath.
- You have a fast heartbeat and your chest hurts.
Seek care immediately if:
- You feel so dizzy that you have trouble standing up.
- Your lips, skin, or nail beds are blue.
Call your doctor or pulmonologist if:
- You have a fever.
- You are lightheaded, dizzy, sweaty, or nauseated after you take your medicine.
- You have more swelling in your legs, feet, or abdomen.
- You are wheezing.
- You cough up bloody sputum.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics help treat an infection caused by bacteria.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Help improve your breathing:
- Go to pulmonary rehabilitation (rehab), if directed. Pulmonary rehab is a program run by specialists to help improve your lung function. The pulmonary rehab team may include doctors, nurses, respiratory therapists, dietitians, and social workers. You may also work with physical and occupational therapists, and psychologists. Pulmonary rehab is usually 3 times per week for a few months.
- Breathing exercises help you breathe more deeply and easily. Do the following if you feel short of breath when you are active:
- Breathe out with pursed or puckered lips (like playing the trumpet).
- Put one hand on your abdomen. Breathe in, causing your hand to move upward. Your lungs will have more room to get bigger and take in more air.
- Oxygen may be needed for a short time. Do not smoke or let anyone else smoke in the same room while your oxygen is on. This may cause a fire. Your healthcare provider will give you more instructions on oxygen use in the home and during travel.
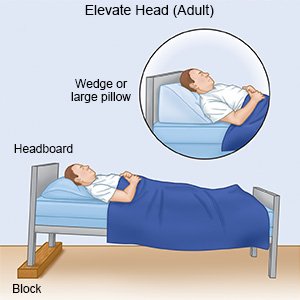
- Elevate your upper body. You may have trouble breathing when you are lying down. Use foam wedges or elevate the head of your bed. This may help you breathe easier while you are resting or sleeping. Use a device that will tilt your whole body, or bend your body at the waist. The device should not bend your body at the upper back or neck.
- Exercise as directed. Your rehab team or your healthcare provider will help you create a long-term exercise plan. Exercise can help your lungs work well, increase muscle strength, and improve your energy level.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Self-care:
- Talk to your healthcare provider about depression. Depression is common after ARDS. You may not have enough energy to do some of the activities you enjoy. You may have muscle weakness that limits your independence. Your healthcare provider can recommend ways to manage or treat depression, if needed.
- Avoid germs. Wash your hands often with soap and water. Use gel hand cleanser when soap and water are not available. Do not touch your eyes, nose, or mouth unless you have washed your hands first. Cover your mouth when you cough. Cough into a tissue or your shirtsleeve so you do not spread germs from your hands. Stay away from others who are sick as much as possible.

- Ask about vaccines. Your risk for lung infections such as pneumonia is higher after ARDS. Get the flu vaccine every year as soon as it becomes available. Get a COVID-19 vaccine and recommended boosters. You may also need the pneumococcal vaccine to prevent pneumonia. Ask your healthcare provider about these or other vaccines you need, and when to get them.
- Eat healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. It may be easier for you to eat several small meals a day rather than a few large meals.

- Do not smoke. Nicotine and other chemicals in cigarettes and cigars increases the risk for lung and heart disease. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Limit or do not drink alcohol as directed. Alcohol can make breathing problems worse. Ask your healthcare provider if alcohol is okay for you to drink. You will need to limit the amount you drink. Your healthcare provider can help you set daily and weekly limits. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
Follow up with your doctor or pulmonologist as directed:
You may need to have the amount of air in your lungs measured as you breathe. This will show how well your lungs are working. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about ARDS
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
