Acute Myeloid Leukemia
Medically reviewed by Drugs.com. Last updated on Jun 5, 2024.
Acute myeloid leukemia (AML) is also called acute myelogenous leukemia. It is a fast-growing cancer of the bone marrow and blood cells. Cells that should become white blood cells (WBCs) do not fully grow. These cells are called myeloblasts and monoblasts. They do not fight infection like a normal WBC should. They crowd the bone marrow and prevent normal blood cells from growing and fighting infection.
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
A heart monitor
is also called an ECG or EKG. Sticky pads placed on your skin record your heart's electrical activity.
A pulse oximeter
is a device that measures the amount of oxygen in your blood. A cord with a clip or sticky strip is placed on your finger, ear, or toe. The other end of the cord is hooked to a machine.
Reverse isolation:
You may be put on reverse isolation safety measures if your body is having a hard time fighting infections. You are given a private room to protect you from other people's germs. Healthcare providers and visitors may wear gloves, a face mask, or a gown to keep their germs away from you. Everyone should wash their hands when entering and leaving your room.
Medicines:
You may be given antibiotics or other medicines to help your body fight infection. You may be given fever or pain medicine, or medicines to relieve nausea or constipation from chemotherapy.
Tests:
- Blood tests are used to count the number of each type of blood cell (RBCs, WBCs, platelets) or to learn more about the kind of AML that you have. You may also need blood tests often while on chemotherapy. These blood tests show how your body is doing and how much chemotherapy medicine is needed.
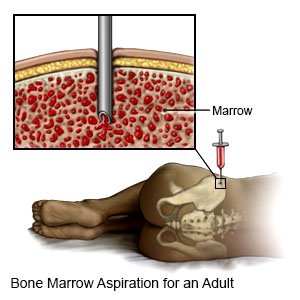
- A bone marrow biopsy is used to take a small amount of bone marrow from the bone in your hip. This test helps healthcare providers find out which type of leukemia you have.
Venous access device:
An IV catheter or tube may be placed in a large vein (blood vessel) near your collarbone, in your neck, or in your arm. You may also have a port, which is a type of venous access device that is placed under the skin and connected to a large vein. You may need a venous access device to receive chemotherapy, other medicines and fluids that need to be given through a big vein. A venous access device can stay in longer than a regular IV can. You may need this device to receive chemotherapy treatments.
Treatment:
Your healthcare provider may first give you treatment to help you go into remission. It may take weeks or months before you go into remission. Your treatment may change if the cancer is not going into remission. After remission, you may need more treatment. Your healthcare provider may give some of the following treatments alone or together:
- Chemotherapy is used to kill cancer cells. You may be more likely to get infections or have other problems after chemotherapy. Healthcare providers will watch you closely and will work with you to decrease the side effects.
- IV fluids are given to help prevent dehydration. It may be difficult for you to drink liquids after chemotherapy starts. Chemotherapy can cause nausea.
- A blood transfusion replaces blood in your body to help it work properly. A blood transfusion is given through an IV. Blood is tested for safety before it is used.
- Bone marrow transplant is used to replace your diseased bone marrow with healthy marrow. The healthy marrow usually comes from someone else. Sometimes your own marrow may be used if it is collected when your cancer is in remission. The bone marrow transplant is given to you in an IV while you are in the hospital.
- Peripheral blood stem cell transplant (PBSCT) is used to put stem cells into your body through an IV. The stem cells go into your bone marrow. Once in the bone marrow, stem cells can grow and become blood cells.
- Radiation kills cancer cells with x-rays or gamma rays. Radiation may be given before you receive a bone marrow or stem cell transplant. You may need radiation if the AML has spread to your spine, brain or other parts of your body.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
Treatment for AML may be slow to work, or may not work at all. AML may not go away or it may return. If you have promyelocytic (M3) leukemia, you may develop retinoic acid syndrome (RAS) from your medicine. RAS can lead to trouble breathing, increased body fluid, and kidney damage. You may be at greater risk for a blood clot in your leg or arm. The blood clot can break loose and travel to your lungs or brain. A blood clot in your lungs can cause chest pain and trouble breathing. A blood clot in your brain can cause a stroke. These problems can be life-threatening.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Acute Myeloid Leukemia
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
