Ticagrelor
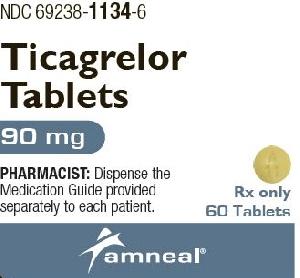
Generic name: ticagrelor [ tye-KA-grel-or ]
Brand names: Brilinta (ticagrelor), Brilinta
Dosage form: oral tablet (60 mg; 90 mg)
Drug class: Platelet aggregation inhibitors
What is ticagrelor?
Ticagrelor is used to lower your risk of heart attack, stroke, or death due to a blocked artery or a prior heart attack.
Ticagrelor is also used to lower your risk of blood clots if you have coronary artery disease (decreased blood flow to the heart) and have been treated with stents to open clogged arteries.
Ticagrelor is also used to lower your risk of a first heart attack or stroke if you have decreased blood flow to the heart.
Ticagrelor is also used to lower the risk of stroke and death in adults with a blockage or decreased blood flow in an artery that supplies blood to the brain.
Ticagrelor is usually given together with low-dose aspirin. Carefully follow your doctor's dosing instructions. Using too much aspirin can make ticagrelor less effective.
Ticagrelor may also be used for purposes not listed in this medication guide.
Ticagrelor side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Ticagrelor may cause serious side effects. Call your doctor at once if you have:
-
slow heartbeats;
-
nosebleeds, or any bleeding that will not stop;
-
shortness of breath even with mild exertion or while lying down;
-
easy bruising, unusual bleeding, purple or red spots under your skin;
-
red, pink, or brown urine;
-
black, bloody, or tarry stools; or
-
coughing up blood or vomit that looks like coffee grounds.
Common side effects of ticagrelor may include:
-
bleeding; or
-
shortness of breath.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Repatha
Repatha (evolocumab) is a PCSK9 inhibitor used to lower high cholesterol alongside dietary changes ...
Wegovy
Wegovy is a once-weekly semaglutide injection used for chronic weight management and to reduce ...
Eliquis
Eliquis (apixaban) is used to reduce the risk of stroke and systemic embolism in patients with ...
Propranolol
Propranolol is a beta-blocker that is used to treat tremors, chest pain, high blood pressure, heart ...
Aspirin
Aspirin is used to treat mild to moderate pain and to reduce fever or inflammation. Learn about ...
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Lisinopril
Lisinopril is an ACE inhibitor. It is used to treat high blood pressure, congestive heart failure ...
Amlodipine
Amlodipine is a calcium channel blocker used to treat high blood pressure and angina by relaxing ...
Warnings
You should not use ticagrelor if you have any active bleeding or a history of bleeding in the brain. Do not use ticagrelor just before heart bypass surgery.
Ticagrelor may cause you to bleed more easily, which can be severe or life-threatening. Call your doctor or seek emergency medical attention if you have bleeding that will not stop, black or bloody stools, red or pink urine, or if you cough up blood or vomit that looks like coffee grounds.
Tell your doctor about all your current medicines and any you start or stop using. Many drugs can interact with ticagrelor.
Do not stop taking ticagrelor without first talking to your doctor, even if you have signs of bleeding. Stopping ticagrelor may increase your risk of a heart attack or stroke.
Before taking this medicine
You should not use ticagrelor if you are allergic to it, or if you have:
-
any active bleeding; or
-
a history of bleeding in the brain (such as from a head injury).
Tell your doctor if you have ever had:
-
a stroke;
-
heart problems;
-
a surgery or bleeding injury;
-
bleeding problems;
-
a stomach ulcer or colon polyps;
-
liver disease; or
-
asthma, COPD (chronic obstructive pulmonary disorder) or other breathing problem.
It is not known whether this medicine will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
You should not breastfeed while using ticagrelor.
How should I take ticagrelor?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Ticagrelor is taken together with aspirin. Use these medicines exactly as directed.
Do not take more aspirin than your doctor has prescribed. Taking too much aspirin can make ticagrelor less effective.
Take ticagrelor at the same times each day, with or without food.
If you cannot swallow a tablet whole, crush the pill and mix it with water. Stir and drink this mixture right away. Add more water to the glass, stir, and drink right away.
Ticagrelor keeps your blood from coagulating (clotting) and can make it easier for you to bleed, even from a minor injury. Contact your doctor or seek emergency medical attention if you have any bleeding that will not stop.
To prevent excessive bleeding, you may need to stop using ticagrelor for a short time before a surgery, medical procedure, or dental work. Any healthcare provider who treats you should know that you are taking ticagrelor.
Do not stop taking ticagrelor without first talking to your doctor, even if you have signs of bleeding. Stopping the medicine could increase your risk of a heart attack or stroke.
ticagrelor may affect medical testing for platelets in your blood and you may have false results. Tell the laboratory staff that you use ticagrelor.
Store at room temperature away from moisture and heat.
What happens if I miss a dose?
Skip the missed dose and use your next dose at the regular time. Do not use two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. Overdose can cause excessive bleeding.
What should I avoid while taking ticagrelor?
Drinking alcohol while taking aspirin can increase your risk of stomach bleeding.
Avoid activities that may increase your risk of bleeding or injury. Use extra care to prevent bleeding while shaving or brushing your teeth.
While taking ticagrelor with aspirin, avoid using medicines for pain, fever, swelling, or cold/flu symptoms. They may contain ingredients similar to aspirin (such as salicylates, ibuprofen, ketoprofen, or naproxen). Taking certain products together can cause you to get too much aspirin which can increase your risk of bleeding.
What other drugs will affect ticagrelor?
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective.
Tell your doctor about all your current medicines. Many drugs can affect ticagrelor, especially:
-
antifungal medicine;
-
antiviral medicine to treat HIV or AIDS;
-
a blood thinner;
-
cholesterol medication;
-
heart or blood pressure medication;
-
opioid medication;
-
seizure medicine; or
-
tuberculosis medicine.
This list is not complete and many other drugs may affect ticagrelor. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Popular FAQ
How long do I have to take Brilinta after a stent or heart attack?
Brilinta is typically used for 6 to 12 months, or longer, after a stent or heart attack. Follow your doctor’s orders when taking Brilinta. It is given with low-dose aspirin to help prevent blood clots. If you stop taking Brilinta too soon, it can increase your risk of a heart attack, stroke or death. Continue reading
What pain medication can I take with Brilinta?
If you take Brilinta, do not take extra aspirin or NSAIDs like ibuprofen, naproxen or celecoxib for pain relief unless directed by your doctor. This may increase your risk for serious bleeding. If you need a mild pain reliever, it is usually safe to take acetaminophen (Tylenol) with Brilinta. Check with your doctor first. Continue reading
How long should Brilinta be held/stopped before surgery?
If you are having surgery, your doctor may instruct you to stop taking Brilinta (ticagrelor) 5 days before your procedure. This will help to lower the chance of bleeding. Always follow your doctor’s directions about when to stop or start taking Brilinta again. Continue reading
More FAQ
- Brilinta vs Plavix: what's the difference?
- Is there a generic for Brilinta?
- Is ticagrelor better than clopidogrel?
- Is ticagrelor a prodrug?
- What is Brilinta (ticagrelor) used for?
More about ticagrelor
- Check interactions
- Compare alternatives
- Reviews (116)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: platelet aggregation inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 5.01.