Seizure
Medically reviewed by Drugs.com. Last updated on Feb 15, 2024.
What is a Seizure?

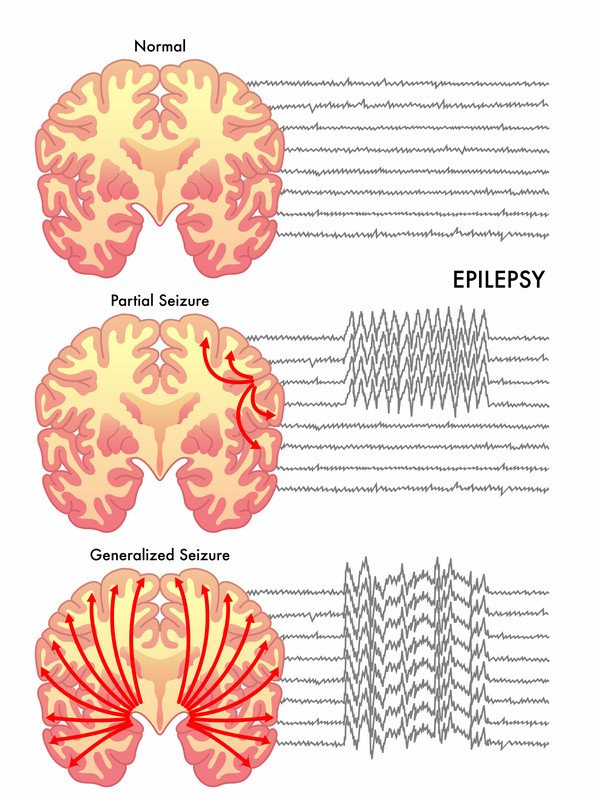
A seizure is a sudden change in the brain's normal electrical activity. During a seizure, brain cells "fire" uncontrollably at up to four times their normal rate, temporarily affecting the way a person behaves, moves, thinks or feels.
There are two major types of seizures:
- Primary generalized seizures – The seizure affects the entire cerebral cortex, the outer portion of the brain that contains the majority of brain cells. In this type of seizure, the abnormal firing of brain cells occurs on both sides of the brain at about the same time.
- Partial (focal) seizure – The abnormal firing of brain cells begins in one region of the brain and remains in that one region.
|
|
Many conditions can affect the brain and trigger a seizure, including:
- Brain injury, either before or after birth
- Infections, especially meningitis and encephalitis
- Eating or drinking toxic substances
- Metabolic problems
- High fever (in children)
- Genetic conditions, including tuberous sclerosis
- Structural abnormalities in the brain's blood vessels
Seizures are common. A person may have only one seizure without a recurrence. Epilepsy is a condition in which seizures continue to recur.
Symptoms
Primary Generalized Seizures
The different types of primary generalized seizures cause different symptoms:
- Generalized tonic-clonic seizure (also called grand mal seizure) – In this type of seizure, the person usually loses consciousness and falls to the ground. All body muscles can contract at once in a sustained contraction, or they can contract in a series of shorter rhythmic contractions, or both. Some patients also lose bowel or bladder control. The seizure episode typically lasts for less than a minute and is followed by period of lethargy (sluggishness) and temporary confusion. Often muscles are very sore after a generalized seizure.
- Absence seizure (also called petit mal seizure) – In this type of seizure, loss of consciousness is so brief that the person usually doesn't change position. For a few seconds, the person may have a blank stare or rapid blinking. This type of seizure usually begins in childhood or early adolescence.
- Status epilepticus – A state of a prolonged seizure (20 minutes or longer) or a series of seizures without fully regaining consciousness. This is a life-threatening medical emergency.
Partial (Focal) Seizures
The different types of partial seizures cause different symptoms:
- Simple partial seizure – In a simple partial seizure, the seizure-related electrical discharges remain localized so that the person experiences a feeling, sensation, movement or other symptom without losing consciousness. During a simple partial seizure, the person remains awake and aware. Symptoms vary depending on the specific brain area involved and may include:
- Jerking movements in one part of the body
- An experience of abnormal smells or a distorted environment
- Unexplained fear or rage
- Complex partial seizure – This is the most common type of partial seizure. In this type of seizure, the person loses awareness of his or her surroundings and is unresponsive or only partially responsive. There may be a blank stare, chewing or lip-smacking, or repetitive movements of the hands. After the seizure, the person typically is confused and has no memory of the episode.
|
|
Either type of partial seizure may become a generalized seizure if the electrical activity spreads from the part of the brain where the seizure started to the rest of the cerebral cortex.
Seizures often are followed by a period of lethargy, drowsiness and confusion. This happens most often with generalized seizures. These symptoms are not part of the seizure itself but are connected to the brain recovering from the effects of the seizure. In addition, warning symptoms called an aura may occur immediately before complex partial and generalized seizures. The aura is actually a brief simple partial seizure that generally involves changes in visual perception, smell, taste or emotional state.
Diagnosis
It's unlikely that you will have seizure symptoms while you are in a doctor's office or emergency department. For this reason, it is important to ask anyone who witnessed your seizure to describe the event and to write it down for your doctor. This description can help your doctor determine the type of seizure you had.
The diagnosis is based primarily on your symptoms that are described. Usually, the physical exam and neurological examination are normal between spells. An adult who experiences a seizure for the first time will be evaluated with a head scan and blood tests to look for chemical imbalances. Your doctor will order either computed tomography (CT) or magnetic resonance imaging (MRI) of the brain. Most people with a new diagnosis of seizure undergo an electroencephalogram (EEG), which monitors and records brain waves from a series of electrodes placed on the scalp. Specific abnormalities in brain wave patterns can help your doctor to determine what kind of seizure you may have. The EEG is a brief outpatient procedure.
|
|
Based on your history and test results, your doctor will decide if he or she has enough information to determine the type of seizure and cause. If not, your doctor may refer you to a neurologist for further evaluation.
Expected Duration
About 5% to 10% of people will have at least one seizure during their lifetimes. For many of these people, the problem is a one-time occurrence that will not return. In about 1 of 10 cases, however, seizures continue to occur, and the person is diagnosed as having epilepsy.
Epilepsy can be a lifelong illness, but many people with a history of multiple seizures eventually will stop having seizures. People who are younger when seizures start and who have a normal neurological examination are more likely to become seizure-free at some point. For people with active epilepsy, the frequency and severity of seizures can be reduced with medication.
Prevention
Epilepsy can be caused by head injury or by any disease that affects the brain. The best way to prevent seizures is to avoid head injury. You can do the following:
- Avoid situations in which a head injury may occur.
- Wear seat belts while driving.
- Equip your car with air bags.
- Wear an approved helmet while skating, riding a motorcycle or bicycling.
- Use protective headgear for sports.
If you have an active seizure disorder, it is also important to take precautions to minimize the risk of injury if you have a seizure. For this reason, it is generally recommended that patients do not operate a motor vehicle or other dangerous machinery until seizures are well controlled. In general, this means waiting for at least six months after the most recent seizure.
Treatment
The primary goal of epilepsy therapy is to prevent seizures as much as possible and minimize side effects.
When seizures are related to an identifiable illness or condition – such as overuse of alcohol or a severe chemical imbalance in the blood – the seizures usually go away when the problem is corrected. When no medical cause for seizures can be found and seizures continue to occur, antiepileptic medications are prescribed. Treatment of epilepsy can be complex. If a single medication doesn't fully control seizures, the next step is usually referral to a neurologist.
Status epilepticus is a life-threatening medical emergency. If not adequately treated, this condition can cause both brain damage and failure of other vital organs. Treatment includes administering antiepileptic medications intravenously (into a vein) until the seizures are controlled.
Antiepileptic medications can cause a variety of side effects, and side effects are more likely to occur with higher doses. Side effects include gastrointestinal upset, elevation of liver enzymes, low white blood cell counts with higher risk of infection, weight gain, drowsiness, confusion and memory problems, dizziness and balance problems, tremor, and double vision.
When medication fails to control a person's seizures, surgery may be considered. The decision to do surgery depends on many factors, including the frequency and severity of seizures, the patient's risk of brain damage or injury from frequent seizures, the effect on quality of life, the patient's overall health, and the likelihood that surgery will control the seizures.
Whether people who have a single, isolated seizure should be treated is controversial. Generally, treatment is recommended for patients who have abnormalities that show up in a neurological examination, brain scan or EEG. These abnormalities increase the chance that the person will have more seizures. Even for people who do not have these abnormalities, there is some evidence that treatment can reduce the risk of more seizures. This possible benefit needs to be balanced against the risk of side effects from medication.
When To Call a Professional
Anyone who has a seizure for the first time needs to be evaluated by a medical professional. For people with epilepsy who have a brief, self-limited seizure, it's not necessary to call a doctor or go to an emergency room following an isolated seizure. However, you should seek emergency care under the after circumstances:
- If the patient does not completely return to his or her normal state after the seizure and post-seizure period, which generally lasts less than 30 to 60 minutes
- If the seizure itself lasts for more than a few minutes
- If the patient has multiple seizures
- If an injury was sustained during the seizure
If you are near a person having a tonic-clonic seizure (grand mal, convulsion), help the person lie down and turn him or her onto one side. Place something soft under the person's head, and loosen tight clothing. Do not restrain the person's arms or legs, and do not put anything into the person's mouth. Forcing something into the mouth may cause more harm than good. The seizure should last less than one to two minutes.
If you are near a person who is having a complex partial seizure, stay with the person, talk calmly, and protect him or her from self-injury. Do not restrain him or her. The person may be able to respond to simple commands, such as, "Sit down." If necessary after the seizure, explain where you are and what has happened.
Prognosis
Seizures that have an identifiable cause (such as a chemical imbalance or overuse of alcohol) usually stop when the medical condition is treated. Many people who have seizures without an identifiable cause eventually will stop having seizures, particularly if seizures begin during childhood. Seizures usually can be well controlled with medication.
Additional Info
Epilepsy Foundation
https://www.epilepsy.com
American Academy of Neurology (AAN)
https://www.aan.com
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.