Warfarin
Generic name: warfarin (oral) [ WAR-far-in ]
Brand names: Coumadin, Jantoven
Drug class: Coumarins and indandiones
What is warfarin?
Warfarin is an anticoagulant (blood thinner). Warfarin reduces the formation of blood clots.
Warfarin is used to treat or prevent blood clots in veins or arteries, which can reduce the risk of stroke, heart attack, or other serious conditions.
Warfarin may also be used for purposes not listed in this medication guide.
Warnings
You should not take warfarin if you are prone to bleeding because of a medical condition, if you have an upcoming surgery, or if you need a spinal tap or epidural. Do not take warfarin if you cannot take it on time every day.
Warfarin increases your risk of severe or fatal bleeding, especially if you have certain medical conditions, if you are 65 or older, or if you have had a stroke, or bleeding in your stomach or intestines. Seek emergency help if you have any bleeding that will not stop.
Call your doctor at once if you have other signs of bleeding such as: swelling, pain, feeling very weak or dizzy, unusual bruising, bleeding gums, nosebleeds, heavy menstrual periods or abnormal vaginal bleeding, blood in your urine, bloody or tarry stools, coughing up blood or vomit that looks like coffee grounds.
Many other drugs can increase your risk of bleeding when used with warfarin. Tell your doctor about all medicines you have recently used.
Avoid making any changes in your diet without first talking to your doctor. Some foods can make warfarin less effective.
Before taking this medicine
You should not take warfarin if you are allergic to it, or if:
-
you have very high blood pressure;
-
you recently had or will have surgery on your brain, spine, or eye;
-
you undergo a spinal tap or spinal anesthesia (epidural); or
-
you cannot take warfarin on time every day.
You also should not take this medicine if you are prone to bleeding because of a medical condition, such as:
-
a blood cell disorder (such as low red blood cells or low platelets);
-
ulcers or bleeding in your stomach, intestines, lungs, or urinary tract;
-
an aneurysm or bleeding in the brain; or
-
an infection of the lining of your heart.
Do not take warfarin if you are pregnant, unless your doctor tells you to. Warfarin can cause birth defects, but preventing blood clots may outweigh any risks to the baby. If you are not pregnant, use effective birth control to prevent pregnancy while taking warfarin and for at least 1 month after your last dose. Tell your doctor right away if you become pregnant.
Warfarin can make you bleed more easily, especially if you have ever had:
-
high blood pressure or serious heart disease;
-
kidney disease;
-
cancer or low blood cell counts;
-
an accident or surgery;
-
bleeding in your stomach or intestines;
-
a stroke; or
-
if you are 65 or older.
To make sure warfarin is safe for you, tell your doctor if you have ever had:
-
diabetes;
-
congestive heart failure;
-
liver disease, kidney disease (or if you are on dialysis);
-
a hereditary clotting deficiency; or
-
low blood platelets after receiving heparin.
It is not known whether warfarin passes into breast milk. Watch for signs of bruising or bleeding in the baby if you take this medicine while you are breast-feeding a baby.
How should I take warfarin?
Take warfarin exactly as prescribed by your doctor. Follow all directions on your prescription label. Your doctor may occasionally change your dose. Do not take warfarin in larger or smaller amounts or for longer than your doctor tells you to.
Take warfarin at the same time every day, with or without food. Never take a double dose.
Warfarin can make it easier for you to bleed. Seek emergency help if you have any bleeding that will not stop.
You will need frequent "INR" or prothrombin time tests (to measure your blood-clotting time and determine your warfarin dose). You must remain under the care of a doctor while taking this medicine.
If you receive warfarin in a hospital, call or visit your doctor 3 to 7 days after you leave the hospital. Your INR will need to be tested at that time. Do not miss any follow-up appointments.
Tell your doctor if you are sick with diarrhea, fever, chills, or flu symptoms, or if your body weight changes.
You may need to stop taking warfarin 5 to 7 days before having any surgery, dental work, or a medical procedure. Call your doctor for instructions.
Wear a medical alert tag or carry an ID card stating that you take warfarin. Any medical care provider who treats you should know that you are taking this medicine.
Store at room temperature away from heat, moisture, and light.
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose can cause excessive bleeding.
What to avoid
Avoid activities that may increase your risk of bleeding or injury. Use extra care to prevent bleeding while shaving or brushing your teeth. You may still bleed more easily for several days after you stop taking warfarin.
Avoid making any changes in your diet without first talking to your doctor. Foods that are high in vitamin K (liver, leafy green vegetables, or vegetable oils) can make warfarin less effective. If these foods are part of your diet, eat a consistent amount on a weekly basis.
Grapefruit juice, cranberry juice, noni juice, and pomegranate juice may interact with warfarin and lead to unwanted side effects. Avoid the use of these juice products while taking this medicine.
Avoid drinking alcohol.
Ask your doctor before using any medicine for pain, arthritis, fever, or swelling. This includes aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib (Celebrex), diclofenac, indomethacin, meloxicam, and others. These medicines may affect blood clotting and may also increase your risk of stomach bleeding.
Warfarin side effects
Get emergency medical help if you have signs of an allergic reaction to warfarin: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Warfarin increases your risk of bleeding, which can be severe or life-threatening. Call your doctor at once if you have any signs of bleeding such as:
-
sudden headache, feeling very weak or dizzy;
-
swelling, pain, unusual bruising;
-
bleeding gums, nosebleeds;
-
bleeding from wounds or needle injections that will not stop;
-
heavy menstrual periods or abnormal vaginal bleeding;
-
blood in your urine, bloody or tarry stools; or
-
coughing up blood or vomit that looks like coffee grounds.
Clots formed by warfarin may block normal blood flow, which could lead to tissue death or amputation of the affected body part. Get medical help at once if you have:
-
pain, swelling, hot or cold feeling, skin changes, or discoloration anywhere on your body; or
-
sudden and severe leg or foot pain, foot ulcer, purple toes or fingers.
Bleeding is the most common side effect of warfarin.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect warfarin?
Many drugs (including some over-the-counter medicines and herbal products) can affect your INR and may increase the risk of bleeding if you take them with warfarin. Not all possible drug interactions are listed in this medication guide. It is very important to ask your doctor and pharmacist before you start or stop using any other medicine, especially:
-
other medicines to prevent blood clots;
-
an antibiotic or antifungal medicine;
-
supplements that contain vitamin K; or
-
herbal (botanical) products - coenzyme Q10, cranberry, echinacea, garlic, ginkgo biloba, ginseng, goldenseal, or St. John's wort.
This list is not complete and many other drugs can interact with warfarin. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Give a list of all your medicines to any healthcare provider who treats you.
Popular FAQ
What is the antidote for warfarin?
Treatment for bleeding associated with warfarin depends upon the level of bleeding, the INR elevation, and risk factors for forming a blood clot. There are several methods to reverse bleeding from warfarin, including vitamin K, prothrombin complex concentrate (PCC), or fresh frozen plasma (FFP). Continue reading
Is warfarin used as rat poison?
Warfarin was the first anticoagulant rodenticide, but today its use is declining as many rodents have grown resistant to it. Rodenticides are pesticides, often formulated into baits, that kill rodents like rats and mice. Continue reading
Does Feverfew interact with any drugs?
Feverfew, an herbal supplement that is a member of the daisy family, may interact with over 40 medicines. This includes drugs used to help prevent blood clots like the anticoagulant warfarin. Continue reading
Why does warfarin cause purple toe syndrome?
Purple toe syndrome is thought to be due to small emboli (blood clots) in the blood vessels which cause a bluish-purple color in the toes and feet. It is a fairly rare complication associated with early warfarin use, usually occurring within the first 3 to 8 weeks of treatment. Continue reading
Does cranberry juice help prevent a UTI?
Cranberry products (concentrated liquid, capsules or tablets) may help to prevent a urinary tract infection (UTI) in some people, but studies have not shown it can help treat an active UTI. Continue reading
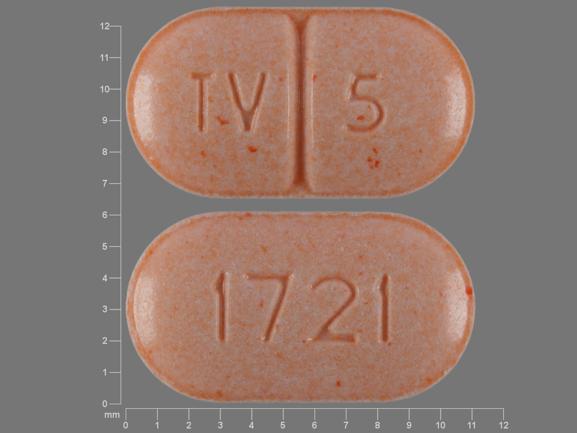
Why are Warfarin tablets color-coded?
Warfarin is color-coded for safety reasons to help prevent medication errors. For example, the 5 milligram (mg) tablet is a light orange color, no matter the manufacturer, but the pill shape and imprints may vary. Continue reading
Is your blood really thinner with warfarin?
When you cut yourself, there is a series of clotting factors found in your blood that help to form a blood clot to stop the bleeding. Warfarin actually blocks (inhibits) these vitamin K-dependent clotting factors and other proteins to keep the blood anti-coagulated, but it does not actually "thin" your blood. Continue reading
References
More about warfarin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (55)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: coumarins and indandiones
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use warfarin only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 24.01.