Ciclomazole: Package Insert / Prescribing Info
Package insert / product label
Generic name: clotrimazole and betamethasone dipropionate, ciclopirox
Dosage form: kit
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Patient Counseling Information
- Warnings
- Precautions
- Storage and Handling
- References
Highlights of Prescribing Information
These highlights do not include all the information needed to use CLOTRIMAZOLE and BETAMETHASONE DIPROPIONATE CREAM safely and effectively. See full prescribing information for CLOTRIMAZOLE and BETAMETHASONE DIPROPIONATE CREAM.
CLOTRIMAZOLE and BETAMETHASONE DIPROPIONATE cream, for topical use Initial U.S. Approval: 1984
Mechanism of Action - The mechanism of action of ciclopirox has been investigated using various in vitro and in vivo infection models. One in vitro study suggested that ciclopirox acts by chelation of polyvalent cations (Fe +3 or Al +3) resulting in the inhibition of the metal-dependent enzymes that are responsible for the degradation of peroxides within the fungal cell. The clinical significance of this observation is not known. (17.1)
Activity in vitro and ex vivo - In vitro methodologies employing various broth or solid media with and without additional nutrients have been utilized to determine ciclopirox minimum inhibitory concentration (MIC) values for the dermatophytic molds. (1-2) As a consequence, a broad range of MIC values, 1-20 ug/mL, were obtained for Trichophyton rubrum and Trichophyton mentagrophytes species. Correlation between in vitro MIC results and clinical outcome has yet to be established for ciclopirox. (17.1)
One ex vivo study was conducted evaluating 8% ciclopirox against new and established Trichophyton rubrum and Trichophyton mentagrophytes infections in ovine hoof material. (3) After 10 days of treatment the growth of T. rubrum and T. mentagrophytes in the established infection model was very minimally affected. Elimination of the molds from hoof material was not achieved in either the new or established infection models. (17.1)
Susceptibility testing for Trichophyton rubrum species - In vitro susceptibility testing methods for determining ciclopirox MIC values against the dermatophytic molds, including Trichophyton rubrum species, have not been standardized or validated. Ciclopirox MIC values will vary depending on the susceptibility testing method employed, composition and pH of media and the utilization of nutritional supplements. Breakpoints to determine whether clinical isolates of Trichophyton rubrum are susceptible or resistant to ciclopirox have not been established. (17.1)
Resistance - Studies have not been conducted to evaluate drug resistance development in T. rubrum species exposed to 8% ciclopirox topical solution. Studies assessing cross-resistance to ciclopirox and other known antifungal agents have not been performed. (17.1)
Antifungal Drug Interactions - No studies have been conducted to determine whether ciclopirox might reduce the effectiveness of systemic antifungal agents for onychomycosis. Therefore, the concomitant use of 8% ciclopirox topical solution and systemic antifungal agents for onychomycosis is not recommended. (17.1)
Pharmacokinetics - As demonstrated in pharmacokinetic studies in animals and man, ciclopirox olamine is rapidly absorbed after oral administration and completely eliminated in all species via feces and urine. Most of the compound is excreted either unchanged or as glucuronide. After oral administration of 10 mg of radiolabeled drug (14C-ciclopirox) to healthy volunteers, approximately 96% of the radioactivity was excreted renally within 12 hours of administration. Ninety-four percent of the renally excreted radioactivity was in the form of glucuronides. Thus, glucuronidation is the main metabolic pathway of this compound. (17.1)
Systemic absorption of ciclopirox was determined in five patients with dermatophytic onychomycoses, after application of ciclopirox topical solution, 8%, to all 20 digits and adjacent 5 mm of skin once daily for six months. Random serum concentrations and 24 hour urinary excretion of ciclopirox were determined at two weeks and at 1, 2, 4 and 6 months after initiation of treatment and four weeks post-treatment. In this study, ciclopirox serum levels ranged from 12-80 ng/mL. Based on urinary data, mean absorption of ciclopirox from the dosage form was <5% of the applied dose. One month after cessation of treatment, serum and urine levels of ciclopirox were below the limit of detection. (17.1)
In two vehicle-controlled trials, patients applied ciclopirox topical solution, 8%, to all toenails and affected fingernails. Out of a total of 66 randomly selected patients on active treatment, 24 had detectable serum ciclopirox concentrations at some point during the dosing interval (range 10.0-24.6 ng/mL). It should be noted that 11 of these 24 patients took concomitant medication containing ciclopirox as ciclopirox olamine. (17.1)
The penetration of the ciclopirox topical solution, 8% was evaluated in an in vitro investigation. Radiolabeled ciclopirox applied once to onychomycotic toenails that were avulsed demonstrated penetration up to a depth of approximately 0.4 mm. As expected, nail plate concentrations decreased as a function of nail depth. The clinical significance of these findings in nail plates is unknown. Nail bed concentrations were not determined. (17.1)
Indications and Usage for Ciclomazole
Clotrimazole and betamethasone dipropionate cream contains a combination of clotrimazole, an azole antifungal, and betamethasone dipropionate, a corticosteroid, and is indicated for the topical treatment of symptomatic inflammatory tinea pedis, tinea cruris, and tinea corporis due to Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton rubrum in patients 17 years and older. ( 1)
Ciclomazole Dosage and Administration
- Tinea pedis: Apply a thin film to the affected skin areas twice a day for 2 weeks. ( 2)
- Tinea cruris and tinea corporis: Apply a thin film to the affected skin area twice a day for 1 week. ( 2)
- Clotrimazole and betamethasone dipropionate cream should not be used longer than 2 weeks in the treatment of tinea corporis or tinea cruris, and longer than 4 weeks in the treatment of tinea pedis. ( 2)
- Do not use with occlusive dressings unless directed by a physician. ( 2)
- Not for ophthalmic, oral or intravaginal use. ( 2)
Dosage Forms and Strengths
Contraindications
None. ( 4)
Warnings and Precautions
- Clotrimazole and betamethasone dipropionate cream can cause reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency during and after withdrawal of the treatment. Risk factor(s) are: use of high-potency topical corticosteroid, use over a large surface area or to areas under occlusion, prolonged use, altered skin barrier, liver failure, and young age. Modify use should HPA axis suppression develop. ( 5.1, 8.4)
- Pediatric patients may be more susceptible to systemic toxicity. ( 5.1, 8.4)
- The use of clotrimazole and betamethasone dipropionate cream in the treatment of diaper dermatitis is not recommended. ( 5.2)
Adverse Reactions/Side Effects
Most common adverse reactions reported for clotrimazole and betamethasone dipropionate cream were paraesthesia in 1.9% of patients and rash, edema, and secondary infections each in less than 1% of patients. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Actavis at 1-800-432-8534 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Indications and Usage for Ciclomazole
(To understand fully the indication for this product, please read the entire INDICATIONS AND USAGE section of the labeling.)
Ciclopirox Topical Solution, 8% as a component of a comprehensive management program, is indicated as topical treatment in immunocompetent patients with mild to moderate onychomycosis of fingernails and toenails without lunula involvement, due to Trichophyton rubrum. The comprehensive management program includes removal of the unattached, infected nails as frequently as monthly, by a health care professional who has special competence in the diagnosis and treatment of nail disorders, including minor nail procedures.
- No studies have been conducted to determine whether ciclopirox might reduce the effectiveness of systemic antifungal agents for onychomycosis. Therefore, the concomitant use of 8% ciclopirox topical solution and systemic antifungal agents for onychomycosis, is not recommended.
- Ciclopirox Topical Solution, 8% should be used only under medical supervision as described above.
- The effectiveness and safety of ciclopirox topical solution, 8% in the following populations has not been studied. The clinical trials with use of ciclopirox topical solution, 8% excluded patients who: were pregnant or nursing, planned to become pregnant, had a history of immunosuppression (e.g., extensive, persistent, or unusual distribution of dermatomycoses, extensive seborrheic dermatitis, recent or recurring herpes zoster, or persistent herpes simplex), were HIV seropositive, received organ transplant, required medication to control epilepsy, were insulin dependent diabetics or had diabetic neuropathy. Patients with severe plantar (moccasin) tinea pedis were also excluded.
- The safety and efficacy of using Ciclopirox Topical Solution, 8% daily for greater than 48 weeks have not been established.
Contraindications
Ciclopirox Topical Solution, 8% is contraindicated in individuals who have shown hypersensitivity to any of its components (19)
Adverse Reactions/Side Effects
In the vehicle-controlled clinical trials conducted in the United States, 9% (30/327) of patients treated with ciclopirox topical solution, 8%, and 7% (23/328) of patients treated with vehicle reported treatment-emergent adverse events (TEAE) considered by the investigator to be causally related to the test material. (22)
The incidence of these adverse events, within each body system, was similar between the treatment groups except for skin and appendages: 8% (27/327) and 4% (14/328) of subjects in the ciclopirox and vehicle groups reported at least one adverse event, respectively. The most common were rash-related adverse events: periungual erythema and erythema of the proximal nail fold were reported more frequently in patients treated with ciclopirox topical solution, 8%, (5% [16/327]) than in patients treated with vehicle (1% [3/328]). Other TEAEs thought to be causally related included nail disorders such as shape change, irritation, ingrown toenail, and discoloration. (22)
The incidence of nail disorders was similar between the treatment groups (2% [6/327] in the ciclopirox topical solution, 8%, group and 2% [7/328] in the vehicle group). Moreover, application site reactions and/or burning of the skin occurred in 1% of patients treated with ciclopirox topical solution, 8%, (3/327) and vehicle (4/328). (22)
A 21-Day Cumulative Irritancy study was conducted under conditions of semi-occlusion. Mild reactions were seen in 46% of patients with the ciclopirox topical solution, 8%, 32% with the vehicle and 2% with the negative control, but all were reactions of mild transient erythema. There was no evidence of allergic contact sensitization for either the ciclopirox topical solution, 8% or the vehicle base. In a separate study of the photosensitization potential of ciclopirox topical solution, 8% in a maximized test design that included the occluded application of sodium lauryl sulfate, no photoallergic reactions were noted. In four subjects localized allergic contact reactions were observed. In the vehicle-controlled studies, one patient treated with ciclopirox topical solution, 8% discontinued treatment due to a rash, localized to the palm (causal relation to test material undetermined). (22)
Use of ciclopirox topical solution, 8% for 48 additional weeks was evaluated in an open-label extension study conducted in patients previously treated in the vehicle-controlled studies. Three percent (9/281) of subjects treated with ciclopirox topical solution, 8% experienced at least one TEAE that the investigator thought was causally related to the test material. Mild rash in the form of periungual erythema (1% [2/281]) and nail disorders (1% [4/281]) were the most frequently reported. Four patients discontinued therapy because of TEAEs. Two of the four had events considered to be related to test material: one patient's great toenail "broke away" and another had an elevated creatine phosphokinase level on Day 1 (after 48 weeks of treatment with the vehicle in the previous vehicle-controlled study). (22)
To report SUSPECTED ADVERSE REACTIONS, contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (22)
See 17 for PATIENT COUNSELING INFORMATION, FDA-approved patient labeling, PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 2/2019
Full Prescribing Information
1. Indications and Usage for Ciclomazole
Clotrimazole and betamethasone dipropionate cream is a combination of an azole antifungal and corticosteroid and is indicated for the topical treatment of symptomatic inflammatory tinea pedis, tinea cruris, and tinea corporis due to Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton rubrum in patients 17 years and older.
2. Ciclomazole Dosage and Administration
Treatment of tinea corporis or tinea cruris:
- Apply a thin film of clotrimazole and betamethasone dipropionate cream into the affected skin areas twice a day for one week.
- Do not use more than 45 grams per week. Do not use with occlusive dressings.
- If a patient shows no clinical improvement after 1 week of treatment with clotrimazole and betamethasone dipropionate cream, the diagnosis should be reviewed.
- Do not use longer than 2 weeks.
Treatment of tinea pedis:
- Gently massage a sufficient amount of clotrimazole and betamethasone dipropionate cream into the affected skin areas twice a day for two weeks.
- Do not use more than 45 grams per week. Do not use with occlusive dressings.
- If a patient shows no clinical improvement after 2 week of treatment with clotrimazole and betamethasone dipropionate cream, the diagnosis should be reviewed.
- Do not use longer than 4 weeks.
Clotrimazole and betamethasone dipropionate cream is for topical use only. It is not for oral, ophthalmic, or intravaginal use.
3. Dosage Forms and Strengths
Cream, 1%/0.05% (base). Each gram of clotrimazole and betamethasone dipropionate cream, USP contains 10 mg of clotrimazole, USP and 0.64 mg of betamethasone dipropionate USP, (equivalent to 0.5 mg of betamethasone) in a white to off-white hydrophilic cream.
5. Warnings and Precautions
5.1 Effects on Endocrine System
Clotrimazole and betamethasone dipropionate cream can cause reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency. This may occur during treatment or after withdrawal of treatment. Cushing’s syndrome and hyperglycemia may also occur due to the systemic effect of corticosteroids while on treatment. Factors that predispose a patient to HPA axis suppression include the use of high-potency steroids, large treatment surface areas, prolonged use, use of occlusive dressing, altered skin barrier, liver failure, and young age.
Because of the potential for systemic corticosteroid effects, patients may need to be periodically evaluated for HPA axis suppression. This may be done by using the adrenocorticotropic hormone (ACTH) stimulation test.
In a small trial, clotrimazole and betamethasone dipropionate cream was applied using large dosages, 7 g daily for 14 days (twice a day) to the crural area of normal adult subjects. Three of the 8 normal subjects on whom clotrimazole and betamethasone dipropionate cream was applied exhibited low morning plasma cortisol levels during treatment. One of these subjects had an abnormal cosyntropin test. The effect on morning plasma cortisol was transient and subjects recovered 1 week after discontinuing dosing. In addition, 2 separate trials in pediatric subjects demonstrated adrenal suppression as determined by cosyntropin testing [see Use in Specific Populations (8.4)].
If HPA axis suppression is documented, gradually withdraw the drug, reduce the frequency of application, or substitute with a less potent corticosteroid.
Pediatric patients may be more susceptible to systemic toxicity due to their larger skin-surface-to-body mass ratios [see Use in Specific Populations (8.4)].
6. Adverse Reactions/Side Effects
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials common adverse reaction reported for clotrimazole and betamethasone dipropionate cream was paresthesia in 1.9% of patients. Adverse reactions reported at a frequency less than 1% included rash, edema, and secondary infection.
6.2 Postmarketing Experience
Because adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following local adverse reactions have been reported with topical corticosteroids: itching, irritation, dryness, folliculitis, hypertrichosis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, maceration of the skin, skin atrophy, striae, miliaria, capillary fragility (ecchymoses), telangiectasia, and sensitization (local reactions upon repeated application of product).
Adverse reactions reported with the use of clotrimazole are: erythema, stinging, blistering, peeling, edema, pruritus, urticaria, and general irritation of the skin.
8. Use In Specific Populations
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C
There are no adequate and well-controlled studies with clotrimazole and betamethasone dipropionate cream in pregnant women. Therefore, clotrimazole and betamethasone dipropionate cream should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
There have been no teratogenic studies performed in animals or humans with the combination of clotrimazole and betamethasone dipropionate. Corticosteroids are generally teratogenic in laboratory animals when administered at relatively low dosage levels.
Studies in pregnant rats with intravaginal doses up to 100 mg/kg (15 times the maximum human dose) revealed no evidence of fetotoxicity due to clotrimazole exposure.
No increase in fetal malformations was noted in pregnant rats receiving oral (gastric tube) clotrimazole doses up to 100 mg/kg/day during gestation Days 6 to 15. However, clotrimazole dosed at 100 mg/kg/day was embryotoxic (increased resorptions), fetotoxic (reduced fetal weights), and maternally toxic (reduced body weight gain) to rats. Clotrimazole dosed at 200 mg/kg/day (30 times the maximum human dose) was maternally lethal, and therefore, fetuses were not evaluated in this group. Also in this study, doses up to 50 mg/kg/day (8 times the maximum human dose) had no adverse effects on dams or fetuses. However, in the combined fertility, teratogenicity, and postnatal development study described above, 50 mg/kg clotrimazole was associated with reduced maternal weight gain and reduced numbers of offspring reared to 4 weeks.
Oral clotrimazole doses of 25, 50, 100, and 200 mg/kg/day (2 to 15 times the maximum human dose) were not teratogenic in mice. No evidence of maternal toxicity or embryotoxicity was seen in pregnant rabbits dosed orally with 60, 120, or 180 mg/kg/day (18 to 55 times the maximum human dose).
Betamethasone dipropionate has been shown to be teratogenic in rabbits when given by the intramuscular route at doses of 0.05 mg/kg. This dose is approximately one-fifth the maximum human dose. The abnormalities observed included umbilical hernias, cephalocele, and cleft palates.
Betamethasone dipropionate has not been tested for teratogenic potential by the dermal route of administration. Some corticosteroids have been shown to be teratogenic after dermal application to laboratory animals.
8.3 Nursing Mothers
Systemically administered corticosteroids appear in human milk and can suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids can result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when clotrimazole and betamethasone dipropionate cream is administered to a nursing woman.
8.4 Pediatric Use
The use of clotrimazole and betamethasone dipropionate cream in patients under 17 years of age is not recommended.
Adverse events consistent with corticosteroid use have been observed in pediatric patients treated with clotrimazole and betamethasone dipropionate cream. In open-label trials, 17 of 43 (39.5%) evaluable pediatric subjects (aged 12 to 16 years old) using clotrimazole and betamethasone dipropionate cream for treatment of tinea pedis demonstrated adrenal suppression as determined by cosyntropin testing. In another open-label trial, 8 of 17 (47.1%) evaluable pediatric subjects (aged 12 to 16 years old) using clotrimazole and betamethasone dipropionate cream for treatment of tinea cruris demonstrated adrenal suppression as determined by cosyntropin testing.
Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA axis suppression when they are treated with topical corticosteroids. They are, therefore also at greater risk of adrenal insufficiency during and/or after withdrawal of treatment. Pediatric patients may be more susceptible than adults to skin atrophy, including striae, when they are treated with topical corticosteroids.
HPA axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in pediatric patients receiving topical corticosteroids [see Warnings and Precautions (5.1)].
Avoid use of clotrimazole and betamethasone dipropionate cream in the treatment of diaper dermatitis.
8.5 Geriatric Use
Clinical studies of clotrimazole and betamethasone dipropionate cream did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. However, greater sensitivity of some older individuals cannot be ruled out. The use of clotrimazole and betamethasone dipropionate cream under occlusion, such as in diaper dermatitis, is not recommended.
Postmarket adverse event reporting for clotrimazole and betamethasone dipropionate cream in patients aged 65 and above includes reports of skin atrophy and rare reports of skin ulceration. Caution should be exercised with the use of these corticosteroid-containing topical products on thinning skin.
11. Ciclomazole Description
Clotrimazole and betamethasone dipropionate cream USP, 1%/0.05% (base), contains combinations of clotrimazole USP, an azole antifungal, and betamethasone dipropionate USP, a corticosteroid, for topical use.
Chemically, clotrimazole, USP is 1-( o-Chloro-α,α-diphenylbenzyl)imidazole, with the molecular formula C 22H 17ClN 2, a molecular weight of 344.84, and the following structural formula:
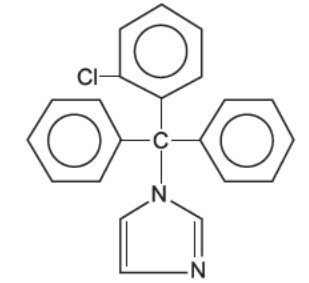
Clotrimazole, USP is an odorless, white crystalline powder, insoluble in water and soluble in ethanol.
Betamethasone dipropionate, USP has 9-Fluoro-11β,17,21-trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 17,21-dipropionate, with the molecular formula C 28H 37FO 7, a molecular weight of 504.59, and the following structural formula:
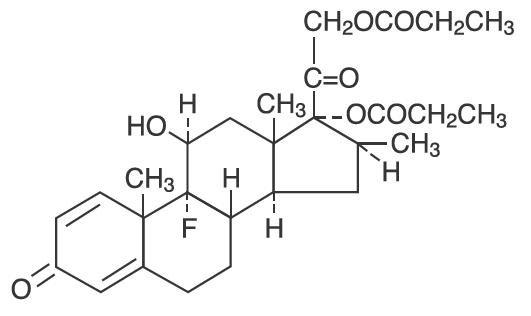
Betamethasone dipropionate, USP is a white to creamy-white, odorless crystalline powder, insoluble in water.
Each gram of clotrimazole and betamethasone dipropionate cream, USP contains 10 mg clotrimazole, USP and 0.64 mg betamethasone dipropionate, USP (equivalent to 0.5 mg betamethasone), in a white to off-white hydrophilic cream. Inactive ingredients: Ceteareth-30, cetyl alcohol, mineral oil, propylene glycol, purified water, sodium phosphate monobasic monohydrate, stearyl alcohol and white petrolatum; benzyl alcohol as preservative.
12. Ciclomazole - Clinical Pharmacology
12.1 Mechanism of Action
Clotrimazole is an azole antifungal [see Clinical Pharmacology (12.4)].
Betamethasone dipropionate is a corticosteroid. Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action for the treatment of tinea pedis, tinea cruris and tinea corporis is unknown.
12.2 Pharmacodynamics
Vasoconstrictor Assay
Studies performed with clotrimazole and betamethasone dipropionate cream indicate that these topical combination antifungal/corticosteroids may have vasoconstrictor potencies in a range that is comparable to high-potency topical corticosteroids. However, similar blanching scores do not necessarily imply therapeutic equivalence.
12.3 Pharmacokinetics
Skin penetration and systemic absorption of clotrimazole and betamethasone dipropionate following topical application of clotrimazole and betamethasone dipropionate cream has not been studied.
The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressings. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin may increase percutaneous absorption of topical corticosteroids. Occlusive dressings substantially increase the percutaneous absorption of topical corticosteroids [see Dosage and Administration (2)] .
Once absorbed through the skin, the pharmacokinetics of topical corticosteroids are similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees. Corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids and their metabolites are also excreted into the bile.
12.4 Microbiology
Mechanism of Action
Clotrimazole, an azole antifungal agent, inhibits 14-α-demethylation of lanosterol in fungi by binding to one of the cytochrome P-450 enzymes. This leads to the accumulation of 14-α-methylsterols and reduced concentrations of ergosterol, a sterol essential for a normal fungal cytoplasmic membrane. The methylsterols may affect the electron transport system, thereby inhibiting growth of fungi.
Activity In Vitro and In Vivo
Clotrimazole has been shown to be active against most strains of the following dermatophytes, both in vitro and in clinical infections, Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton rubrum [see Indications and Usage (1)].
Drug Resistance
Strains of dermatophytes having a natural resistance to clotrimazole have not been reported. Resistance to azoles, including clotrimazole, has been reported in some Candida species.
No single-step or multiple-step resistance to clotrimazole has developed during successive passages of Trichophyton mentagrophytes.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
There are no adequate laboratory animal studies with either the combination of clotrimazole and betamethasone dipropionate or with either component individually to evaluate carcinogenesis.
Betamethasone was negative in the bacterial mutagenicity assay ( Salmonella typhimurium and Escherichia coli) and in the mammalian cell mutagenicity assay (CHO/HGPRT). It was positive in the in vitro human lymphocyte chromosome aberration assay, and equivocal in the in vivo mouse bone marrow micronucleus assay.
Reproductive studies with betamethasone dipropionate carried out in rabbits at doses of 1 mg/kg by the intramuscular route and in mice up to 33 mg/kg by the intramuscular route indicated no impairment of fertility except for dose-related increases in fetal resorption rates in both species. These doses are approximately 5- and 38-fold the maximum human dose based on body surface areas, respectively.
In a combined study of the effects of clotrimazole on fertility, teratogenicity, and postnatal development, male and female rats were dosed orally (diet admixture) with levels of 5, 10, 25, or 50 mg/kg/day (approximately 1 to 8 times the maximum dose in a 60-kg adult based on body surface area) from 10 weeks prior to mating until 4 weeks postpartum. No adverse effects on the duration of estrous cycle, fertility, or duration of pregnancy were noted.
14. Clinical Studies
In clinical trials of tinea corporis, tinea cruris, and tinea pedis, subjects treated with clotrimazole and betamethasone dipropionate cream showed a better clinical response at the first return visit than subjects treated with clotrimazole cream. In tinea corporis and tinea cruris, the subject returned 3 to 5 days after starting treatment, and in tinea pedis, after 1 week. Mycological cure rates observed in subjects treated with clotrimazole and betamethasone dipropionate cream were as good as, or better than, in those subjects treated with clotrimazole cream. In these same clinical studies, patients treated with clotrimazole and betamethasone dipropionate cream showed better clinical responses and mycological cure rates when compared with subjects treated with betamethasone dipropionate cream.
16. How is Ciclomazole supplied
Clotrimazole and betamethasone dipropionate cream, USP is available as follows:
15 gram tube in a carton (NDC 0472-0379-15)
45 gram tube in a carton (NDC 0472-0379-45)
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature].
17. Patient Counseling Information
See FDA-Approved Patient Labeling ( Patient Information)
Inform the patient of the following:
- Use clotrimazole and betamethasone dipropionate cream as directed by the physician. It is for external use only.
- Avoid contact with the eyes, the mouth, or intravaginally.
- Do not use clotrimazole and betamethasone dipropionate cream on the face or underarms.
- Do not use more than 45 grams of clotrimazole and betamethasone dipropionate cream per week.
- When using clotrimazole and betamethasone dipropionate cream in the groin area, patients should use the medication for 2 weeks only, and apply the cream sparingly. Patients should wear loose-fitting clothing. Notify the physician if the condition persists after 2 weeks.
- Do not use clotrimazole and betamethasone dipropionate cream for any disorder other than that for which it was prescribed.
- Do not bandage, cover or wrap the treatment area unless directed by the physician. Avoid use of clotrimazole and betamethasone dipropionate cream in the diaper area, as diapers or plastic pants may constitute occlusive dressing.
- Report any signs of local adverse reactions to the physician. Advise patients that local reactions and skin atrophy are more likely to occur with occlusive use or prolonged use.
- This medication is to be used for the full prescribed treatment time, even though the symptoms may have improved. Notify the physician if there is no improvement after 1 week of treatment for tinea cruris or tinea corporis, or after 2 weeks for tinea pedis.
Manufactured by:
G&W Laboratories, Inc.
111 Coolidge Street
South Plainfield, NJ 07080 USA
Distributed by:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
I600-5511/14A GW7100
Revised – July 2016
PATIENT INFORMATION
Clotrimazole (kloe trim' a zole) and
Betamethasone Dipropionate (bay" ta meth' a sone dye proe' pee oh nate)
Cream USP, 1%/0.05% (base)
Important information: Clotrimazole and betamethasone dipropionate cream is for use on skin only. Do not use clotrimazole and betamethasone dipropionate cream in your eyes, mouth, or vagina.
What is clotrimazole and betamethasone dipropionate cream?
- Clotrimazole and betamethasone dipropionate cream is a prescription medication used on the skin (topical) to treat fungal infections of the feet, groin, and body in people 17 years of age and older. Clotrimazole and betamethasone dipropionate cream is used for fungal infections that are inflamed and have symptoms of redness or itching.
- Clotrimazole and betamethasone dipropionate cream should not be used in children under 17 years of age.
Before using clotrimazole and betamethasone dipropionate cream, tell your healthcare provider about all your medical conditions, including if you:
- are pregnant or plan to become pregnant. It is not known if clotrimazole and betamethasone dipropionate cream will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if clotrimazole and betamethasone dipropionate passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take other corticosteroid medicines by mouth or use other products on your skin or scalp that contain corticosteroids.
What should I avoid while using clotrimazole and betamethasone dipropionate cream?
Clotrimazole and betamethasone dipropionate cream should not be used to treat diaper rash or redness. You should avoid applying clotrimazole and betamethasone dipropionate cream in the diaper area.
How should I use clotrimazole and betamethasone dipropionate cream?
- Use clotrimazole and betamethasone dipropionate cream exactly as your healthcare provider tells you to use it.
- Use clotrimazole and betamethasone dipropionate cream for the prescribed treatment time, even if your symptoms get better.
- Do not use more than 45 grams of clotrimazole and betamethasone dipropionate cream in 1 week.
- Do not bandage, cover, or wrap the treated area unless your healthcare provider tells you to. Wear loose-fitting clothing if you use clotrimazole and betamethasone dipropionate cream in the groin area.
- Do not use clotrimazole and betamethasone dipropionate cream on your face or underarms (armpits).
-
For treatment of fungal infections of the groin and body:
- Apply a thin layer of clotrimazole and betamethasone dipropionate cream to the affected skin area 2 times a day for 1 week.
- Tell your healthcare provider if the treated skin area does not improve after 1 week of treatment.
- Do not use clotrimazole and betamethasone dipropionate cream for longer than 2 weeks.
-
For treatment of fungal infections of the feet:
- Apply a thin layer of clotrimazole and betamethasone dipropionate cream to the affected skin area 2 times a day for 2 weeks.
- Tell your healthcare provider if the treated skin area does not improve after 2 weeks of treatment. Do not use clotrimazole and betamethasone dipropionate cream longer than 4 weeks.
- Wash your hands after applying clotrimazole and betamethasone dipropionate cream.
What are the possible side effects of clotrimazole and betamethasone dipropionate cream?
Clotrimazole and betamethasone dipropionate cream may cause serious side effects, including:
- Clotrimazole and betamethasone dipropionate cream can pass through your skin. Too much clotrimazole and betamethasone dipropionate cream passing through your skin can cause your adrenal glands to stop working. Your healthcare provider may do blood tests to check for adrenal gland problems.
The most common side effects of clotrimazole and betamethasone dipropionate cream include burning, tingling, rash, swelling, and infections.
These are not all the possible side effects of clotrimazole and betamethasone dipropionate cream.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store clotrimazole and betamethasone dipropionate cream?
- Store clotrimazole and betamethasone dipropionate cream at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep clotrimazole and betamethasone dipropionate cream and all medicines out of the reach of children.
General information about the safe and effective use of clotrimazole and betamethasone dipropionate cream.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. You can ask your pharmacist or healthcare provider for information about clotrimazole and betamethasone dipropionate cream that is written for health professionals. Do not use clotrimazole and betamethasone dipropionate cream for a condition for which it was not prescribed. Do not give clotrimazole and betamethasone dipropionate cream to other people, even if they have the same symptoms that you have. It may harm them.
What are the ingredients in clotrimazole and betamethasone dipropionate cream?
Active ingredients: clotrimazole, USP and betamethasone dipropionate, USP
Inactive ingredients: Ceteareth-30, cetyl alcohol, mineral oil, propylene glycol, purified water, sodium phosphate monobasic monohydrate, stearyl alcohol and white petrolatum; benzyl alcohol as preservative.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Manufactured by:
G&W Laboratories, Inc.
111 Coolidge Street
South Plainfield, NJ 07080 USA
Distributed by:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
I600-5511/14A GW7100
Revised – July 2016
Ciclopirox Topical Solution, 8% Nail Lacquer Rx Only For use on fingernails and toenails and immediately adjacent skin only. Not for use in eyes.
Ciclomazole Description
Ciclopirox Topical Solution, 8% contains a synthetic antifungal agent, ciclopirox. It is intended for topical use on fingernails and toenails and immediately adjacent skin.
Each gram of Ciclopirox Topical Solution, 8% contains 80 mg ciclopirox in a solution base consisting of butyl ester of poly [vinylmethylether/maleic acid copolymer] in isopropyl alcohol, ethyl acetate, and isopropyl alcohol. Ethyl acetate and isopropyl alcohol are solvents that vaporize after application.
Ciclopirox Topical Solution, 8% is a clear, colorless to the slightly yellowish solution.
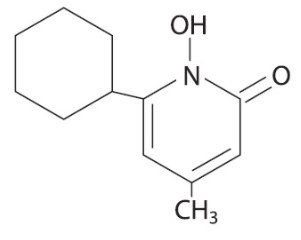
The chemical name for ciclopirox is 6-cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridone, with the empirical formula C 12H 17NO 2 and a molecular weight of 207.27.
The CAS Registry Number is [29342-05-0]. The chemical structure is:
Ciclomazole - Clinical Pharmacology
Clinical Trials Data -
The results of use of ciclopirox topical solution, 8% in treatment of onychomycosis of the toenail without lunula involvement were obtained from two double-blind, placebo-controlled studies conducted in the United States. In these studies, patients with onychomycosis of the great toenails without lunula involvement were treated with ciclopirox topical solution, 8% in conjunction with monthly removal of the unattached, infected toenail by the investigator. Ciclopirox topical solution, 8%, was applied for 48 weeks. At baseline, patients had 20–65% involvement of the target great toenail plate. Statistical significance was demonstrated in one of two studies for the endpoint "complete cure" (clear nail and negative mycology), and in two studies for the endpoint "almost clear" (≤10% nail involvement and negative mycology) at the end of study. These results are presented below.
|
At Week 48 (plus Last Observation Carried Forward) for the Intent-to-Treat (ITT) Population |
||||
|
Study 312 |
Study 313 |
|||
|
Active |
Vehicle |
Active |
Vehicle |
|
|
Complete Cure* |
6/110 (5.5%) |
1/109 (0.9%) |
10/118 (8.5%) |
0/117 (0%) |
|
Almost Clear** |
7/107 (6.5%) |
1/108 (0.9%) |
14/116 (12%) |
1/115 (0.9%) |
|
Negative Mycology Alone*** |
30/105 (29%) |
12/106 (11%) |
41/115 (36%) |
10/114 (9%) |
|
* Clear nail and negative mycology ** ≤ 10% nail involvement and negative mycology *** Negative KOH and negative culture |
||||
The summary of reported patient outcomes for the ITT population at 12 weeks following the end of treatment are presented below. Note that post-treatment efficacy assessments were scheduled only for patients who achieved a complete cure.
|
Post-Treatment Week 12 Data for Patients Who Achieved Complete Cure at Week 48 |
||||
|
Study 312 |
Study 313 |
|||
|
Active |
Vehicle |
Active |
Vehicle |
|
|
Number of Treated Patients |
112 |
111 |
119 |
118 |
|
Complete Cure at Week 48 |
6 |
1 |
10 |
0 |
|
Post-treatment Week 12 Outcomes: | ||||
|
Patients Missing All Week 12 Assessments |
2 |
0 |
2 |
0 |
|
Patients with Week 12 Assessments |
4 |
1 |
8 |
0 |
|
Complete Cure |
3 |
1 |
4 |
0 |
|
Almost Clear |
2* |
1 |
1* |
0 |
|
Negative Mycology |
3 |
1 |
5 |
0 |
*Four patients (from studies 312 and 313) who were completely cured did not have post-treatment Week 12 planimetry data.
Warnings
Ciclopirox Topical Solution, 8% is not for ophthalmic, oral, or intravaginal use. It is for use on nails and immediately adjacent skin only.
Precautions
If a reaction suggesting sensitivity or chemical irritation should occur with the use of Ciclopirox Topical Solution, 8% treatment should be discontinued and appropriate therapy instituted. So far there is no relevant clinical experience with patients with insulin-dependent diabetes or who have diabetic neuropathy. The risk of removal of the unattached, infected nail, by the health care professional and trimming by the patient, should be carefully considered before prescribing to patients with a history of insulin-dependent diabetes mellitus or diabetic neuropathy.
Information for Patients
Patients should have detailed instructions regarding the use of Ciclopirox Topical Solution, 8% as a component of a comprehensive management program for onychomycosis in order to achieve maximum benefit with the use of this product.
The patient should be told to:
1. Use Ciclopirox Topical Solution, 8% as directed by a health care professional. Avoid contact with the eyes and mucous membranes. Contact with skin other than skin immediately surrounding the treated nail(s) should be avoided. Ciclopirox Topical Solution, 8% is for external use only.
2. Ciclopirox Topical Solution, 8% should be applied evenly over the entire nail plate and 5 mm of surrounding skin. If possible, Ciclopirox Topical Solution, 8% should be applied to the nail bed, hyponychium, and the undersurface of the nail plate when it is free of the nail bed (e.g., onycholysis). Contact with the surrounding skin may produce mild, transient irritation (redness).
3. Removal of the unattached, infected nail, as frequently as monthly, by a health care professional is needed with use of this medication. Inform a health care professional if they have diabetes or problems with numbness in the toes or fingers for consideration of the appropriate nail management program.
4. Inform a health care professional if the area of application shows signs of increased irritation (redness, itching, burning, blistering, swelling, or oozing).
5. Up to 48 weeks of daily applications with Ciclopirox Topical Solution, 8% and professional removal of the unattached, infected nail, as frequently as monthly, are considered the full treatment needed to achieve a clear or almost clear nail (defined as 10% or less residual nail involvement).
6. Six months of therapy with professional removal of the unattached, infected nail may be required before initial improvement of symptoms is noticed.
7. A completely clear nail may not be achieved with use of this medication. In clinical studies less than 12% of patients were able to achieve either a completely clear or almost clear toenail.
8. Do not use the medication for any disorder other than that for which it is prescribed.
9. Do not use nail polish or other nail cosmetic products on the treated nails.
10. Avoid use near heat or open flame, because product is flammable.
Carcinogenesis, Mutagenesis, Impairment of Fertility -
No carcinogenicity study was conducted with ciclopirox topical solution, 8% formulation. A carcinogenicity study of ciclopirox (1% and 5% solutions in polyethylene glycol 400) in female mice dosed topically twice per week for 50 weeks followed by a six-month drug-free observation period prior to necropsy revealed no evidence of tumors at the application sites. In human systemic tolerability studies following daily application (~340 mg of ciclopirox topical solution, 8%) in subjects with distal subungual onychomycosis, the average maximal serum level of ciclopirox was 31±28 ng/mL after two months of once daily applications. This level was 159 times lower than the lowest toxic dose and 115 times lower than the highest nontoxic dose in rats and dogs fed 7.7 and 23.1 mg ciclopirox (as ciclopirox olamine)/kg/day.
The following in vitro genotoxicity tests have been conducted with ciclopirox: evaluation of gene mutation in Ames Salmonella and E. coli assays (negative); chromosome aberration assays in V79 Chinese hamster lung fibroblasts, with and without metabolic activation (positive); gene mutation assay in the HGPRT-test with V79 Chinese hamster lung fibroblasts (negative); unscheduled DNA synthesis in human A549 cells (negative); and BALB/c3T3 cell transformation assay (negative). In an in vivo Chinese hamster bone marrow cytogenetic assay, ciclopirox was negative for chromosome aberrations at 5,000 mg/kg.
The following in vitro genotoxicity tests were conducted with ciclopirox topical solution, 8%: Ames Salmonella test (negative); unscheduled DNA synthesis in the rat hepatocytes (negative); cell transformation assay in BALB/c3T3 cell assay (positive). The positive response of the lacquer formulation in the BALB/c3T3 test was attributed to its butyl monoester of poly[methylvinyl ether/maleic acid] resin component (Gantrez® ES-435), which also tested positive in this test. The cell transformation assay may have been confounded because of the film-forming nature of the resin.
Gantrez® ES-435 tested nonmutagenic in both the in vitro mouse lymphoma forward mutation assay with or without activation and unscheduled DNA synthesis assay in rat hepatocytes.
Oral reproduction studies in rats at doses up to 3.85 mg ciclopirox (as ciclopirox olamine)/kg/day [equivalent to approximately 1.4 times the potential exposure at the maximum recommended human topical dose (MRHTD)] did not reveal any specific effects on fertility or other reproductive parameters. MRHTD (mg/m2) is based on the assumption of 100% systemic absorption of 27.12 mg ciclopirox (~340 mg ciclopirox topical solution, 8%) that will cover all the fingernails and toenails including 5 mm proximal and lateral fold area plus onycholysis to a maximal extent of 50%.
Pregnancy:
Teratogenic Effects:
Pregnancy Category B -
Teratology studies in mice, rats, rabbits, and monkeys at oral doses of up to 77, 23, 23, or 38.5 mg, respectively, of ciclopirox as ciclopirox olamine/kg/day (14, 8, 17, and 28 times MRHTD), or in rats and rabbits receiving topical doses of up to 92.4 and 77 mg/kg/day, respectively (33 and 55 times MRHTD), did not indicate any significant fetal malformations.
There are no adequate or well-controlled studies of topically applied ciclopirox in pregnant women. Ciclopirox Topical Solution, 8% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers -
It is not known whether this drug is excreted in human milk. Since many drugs are excreted in human milk, caution should be exercised when Ciclopirox Topical Solution, 8% is administered to a nursing woman.
Pediatric Use -
Based on the safety profile in adults, Ciclopirox Topical Solution, 8% is considered safe for use in children 12 years and older. No clinical trials have been conducted in the pediatric population.
Geriatric Use -
Clinical studies of ciclopirox topical solution, 8% did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between elderly and younger patients.
Adverse Reactions/Side Effects
In the vehicle-controlled clinical trials conducted in the United States, 9% (30/327) of patients treated with ciclopirox topical solution, 8%, and 7% (23/328) of patients treated with vehicle reported treatment-emergent adverse events (TEAE) considered by the investigator to be causally related to the test material.
The incidence of these adverse events, within each body system, was similar between the treatment groups except for skin and appendages: 8% (27/327) and 4% (14/328) of subjects in the ciclopirox and vehicle groups reported at least one adverse event, respectively. The most common were rash-related adverse events: periungual erythema and erythema of the proximal nail fold were reported more frequently in patients treated with ciclopirox topical solution, 8%, (5% [16/327]) than in patients treated with vehicle (1% [3/328]). Other TEAEs thought to be causally related included nail disorders such as shape change, irritation, ingrown toenail, and discoloration.
The incidence of nail disorders was similar between the treatment groups (2% [6/327] in the ciclopirox topical solution, 8%, group and 2% [7/328] in the vehicle group). Moreover, application site reactions and/or burning of the skin occurred in 1% of patients treated with ciclopirox topical solution, 8%, (3/327) and vehicle (4/328).
A 21-Day Cumulative Irritancy study was conducted under conditions of semi-occlusion. Mild reactions were seen in 46% of patients with the ciclopirox topical solution, 8%, 32% with the vehicle and 2% with the negative control, but all were reactions of mild transient erythema. There was no evidence of allergic contact sensitization for either the ciclopirox topical solution, 8% or the vehicle base. In a separate study of the photosensitization potential of ciclopirox topical solution, 8% in a maximized test design that included the occluded application of sodium lauryl sulfate, no photoallergic reactions were noted. In four subjects localized allergic contact reactions were observed. In the vehicle-controlled studies, one patient treated with ciclopirox topical solution, 8% discontinued treatment due to a rash, localized to the palm (causal relation to test material undetermined).
Use of ciclopirox topical solution, 8% for 48 additional weeks was evaluated in an open-label extension study conducted in patients previously treated in the vehicle-controlled studies. Three percent (9/281) of subjects treated with ciclopirox topical solution, 8% experienced at least one TEAE that the investigator thought was causally related to the test material. Mild rash in the form of periungual erythema (1% [2/281]) and nail disorders (1% [4/281]) were the most frequently reported. Four patients discontinued therapy because of TEAEs. Two of the four had events considered to be related to test material: one patient's great toenail "broke away" and another had an elevated creatine phosphokinase level on Day 1 (after 48 weeks of treatment with the vehicle in the previous vehicle-controlled study).
To report SUSPECTED ADVERSE REACTIONS, contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Ciclomazole Dosage and Administration
Ciclopirox Topical Solution, 8% should be used as a component of a comprehensive management program for onychomycosis. Removal of the unattached, infected nail, as frequently as monthly, by a health care professional, weekly trimming by the patient, and daily application of the medication are all integral parts of this therapy. Careful consideration of the appropriate nail management program should be given to patients with diabetes (see PRECAUTIONS).
Nail Care By Health Care Professionals - Removal of the unattached, infected nail, as frequently as monthly, trimming of onycholytic nail, and filing of excess horny material should be performed by professionals trained in treatment of nail disorders.
Nail Care By Patient – Patients should file away (with emery board) loose nail material and trim nails, as required, or as directed by the health care professional, every seven days after Ciclopirox Topical Solution, 8% is removed with alcohol.
Ciclopirox Topical Solution, 8% should be applied once daily (preferably at bedtime or eight hours before washing) to all affected nails with the applicator brush provided. Ciclopirox Topical Solution, 8% should be applied evenly over the entire nail plate.
If possible, Ciclopirox Topical Solution, 8% should be applied to the nail bed, hyponychium, and the under surface of the nail plate when it is free of the nail bed (e.g., onycholysis).
Ciclopirox Topical Solution, 8% should not be removed on a daily basis. Daily applications should be made over the previous coat and removed with alcohol every seven days. This cycle should be repeated throughout the duration of therapy.
How is Ciclomazole supplied
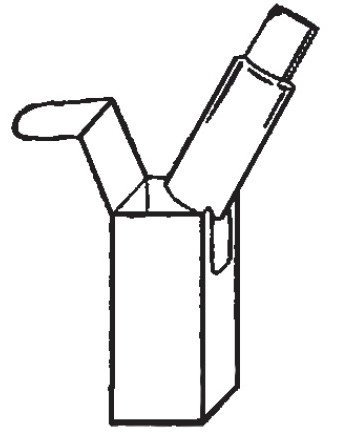
Ciclopirox Topical Solution, 8% is available as follows:
6.6 mL glass bottle with a screw cap fitted with a brush (NDC 45802- 141-67)
References
1.Dittmar W., Lohaus G. 1973. HOE296, A new antimycotic compound with a broad antimicrobial spectrum. Arzneim-Forsch./ Drug Res. 23:670-674.
2.Niewerth et. al., 1998. Antimicrobial susceptibility testing of dermatophytes:
Comparison of the agar macrodilution and broth microdilution tests. Chemotherapy. 44:31-35.
3.Yang et. al. 1997. A new simulation model for studying in vitro topical penetration of antifungal drugs into hard keratin. J. Mycol. Med. 7:195-98.
Patient Instructions
Ciclopirox Topical Solution, 8%
Nail Lacquer
Rx Only
Patient Information and Instructions
Patients should have detailed instructions regarding the use of Ciclopirox Topical Solution, 8% as a component of a comprehensive management program for onychomycosis in order to achieve maximum benefit with the use of this product. Discuss your treatment plan with your health care professional for regular removal of the unattached, infected nail.
Before using this medication, tell your doctor if you:
- Are pregnant or nursing
- Are you an insulin-dependent diabetic or have diabetic neuropathy
- Have a history of immunosuppression
- Are immunocompromised (e.g., received an organ transplant, etc.)
- Require medication to control epilepsy
- Use or require topical corticosteroids on a repeated monthly basis
- Use steroid inhalers on a regular basis
Patient Information:
- Use Ciclopirox Topical Solution, 8% as directed by your health care professional.
- Ciclopirox Topical Solution, 8% is for external use only.
- Contact with skin other than skin immediately surrounding the treated nail(s) should be avoided.
- Avoid contact with the eyes and mucous membranes.
- Removal of the unattached, infected nail, as frequently as monthly, by your health care professional is needed with the use of this medication to obtain maximal benefit with the use of this product. If you have diabetes or problems with numbness in your toes or fingers, talk to your health care provider before trimming your nails or removing any nail material.
- Inform your health care professional if the area of application shows signs of increased irritation (redness, itching, burning, blistering, swelling, or oozing).
- Up to 48 weeks of daily applications with Ciclopirox Topical Solution, 8% and professional removal, as frequently as monthly, of the unattached, infected nail are considered the full treatment time to achieve a clear or almost clear nail (defined as 10% or less residual nail involvement). Six months of therapy with professional removal of the unattached, infected nail may be required before initial improvement of symptoms is noticed.
- A completely clear nail may not be achieved with the use of this medication. In clinical studies, less than 12% of patients were able to achieve either a clear or almost clear toenail.
- Do not use nail polish or other nail cosmetic products on the treated nails.
- Avoid use near heat or open flame, because the product is flammable.
Patient Instructions
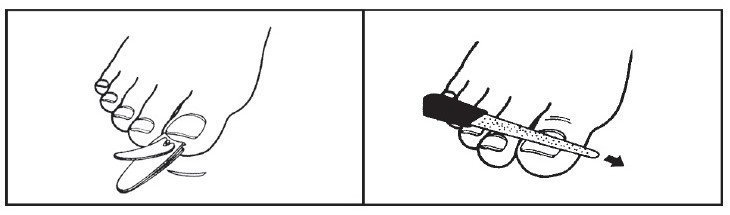
1- Before starting treatment, remove any loose nail or nail material using scissors, nail clippers or a nail file. If you have diabetes or problems with numbness in your toes or fingers, talk to your health care provider before trimming your nails or removing any nail material.
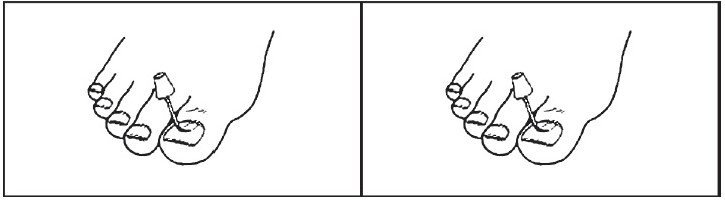
2- Apply Ciclopirox Topical Solution, 8% once daily (preferably at bedtime) to all affected nails with the applicator brush provided. Apply the lacquer evenly over the entire nail. Where possible, nail lacquer should also be applied to the underside of the nail and to the skin beneath it. Allow lacquer to dry (approximately 30 seconds) before putting on socks or stockings. After applying the medication, wait eight hours before taking a bath or shower.
3- Apply Ciclopirox Topical Solution, 8% daily over the previous coat.
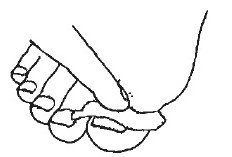
4- Once a week, remove the Ciclopirox Topical Solution, 8% with alcohol. Remove as much of the damaged nail as possible using scissors, nail clippers, or a nail file.
5- Repeat process (steps 2 through 4).
Please Note:
- To prevent the screw cap from sticking to the bottle, do not allow the solution to get into the bottle threads.
- To prevent the solution from drying out, the bottle should be closed tightly after every use.
- To protect from light, replace the bottle in the carton after each use.
Manufactured By
Perrigo
Bronx, NY 10457
Distributed By
Perrigo®
Allegan, MI 49010
Rev 02-17
: 3C000 RC J6
| CICLOMAZOLE
clotrimazole and betamethasone dipropionate, ciclopirox kit |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| Labeler - PureTek Corporation (785961046) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| PERRIGO NEW YORK INC | 078846912 | manufacture(45802-141) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| G&W NC Laboratories, LLC | 079419931 | manufacture(0472-0379) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| PureTek Corporation | 785961046 | pack(59088-769) | |