Tisagenlecleucel (Monograph)
Brand name: Kymriah
Drug class: Gene Therapy
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for tisagenlecleucel to ensure that the benefits outweigh the risks. The REMS may apply to one or more preparations of tisagenlecleucel and consists of the following: elements to assure safe use and implementation system. See REMS under Cautions and also see the FDA REMS page ([Web]).
Posted 11/28/2023
The Food and Drug Administration (FDA) has received reports of T-cell malignancies, including chimeric antigen receptor CAR-positive lymphoma, in patients who received treatment with BCMA- or CD19-directed autologous CAR T cell immunotherapies. Reports were received from clinical trials and/or postmarketing adverse event (AE) data sources.
FDA has determined that the risk of T-cell malignancies is applicable to all currently approved BCMA-directed and CD19-directed genetically modified autologous CAR T cell immunotherapies. T-cell malignancies have occurred in patients treated with several products in the class.
Although the overall benefits of these products continue to outweigh their potential risks for their approved uses, FDA is investigating the identified risk of T cell malignancy with serious outcomes, including hospitalization and death, and is evaluating the need for regulatory action.
For more information visit the FDA website at: [Web].
Warning
WARNING: CYTOKINE RELEASE SYNDROME and NEUROLOGICAL TOXICITIES
See full prescribing information for complete boxed warning.
-
Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving tisagenlecleucel. Do not administer tisagenlecleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.
-
Neurological toxicities, which may be severe or life-threatening, can occur following treatment with tisagenlecleucel, including concurrently with CRS. Monitor for neurological events after treatment with tisagenlecleucel. Provide supportive care as needed.
-
Tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Kymriah REMS.
Introduction
Tisagenlecleucel is a CD19-directed genetically modified autologous T-cell immunotherapy.
Uses for Tisagenlecleucel
Tisagenlecleucel has the following uses:
Tisagenlecleucel is a chimeric antigen receptor (CAR) T-cell therapy with the following indications:
Treatment of pediatric patients and young adults up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. Designated an orphan drug by FDA for this indication. Efficacy of tisagenlecleucel for this use was evaluated in an open-label, multicenter, single-arm trial (ELIANA) in patients 3–23 years of age with refractory or relapsed (r/r) B-cell precursor ALL. Treatment consisted of lymphodepleting chemotherapy (fludarabine and cyclophosphamide) followed by a single IV infusion of tisagenlecleucel. Among 63 evaluable patients, 83% achieved complete remission or complete remission with incomplete blood count recovery, all of which were minimal residual disease (MRD)-negative, within 3 months after infusion. The median duration of remission was not reached at a median follow-up of 4.8 months.
Treatment of adults with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. Tisagenlecleucel is not indicated for treatment of patients with primary CNS lymphoma. Designated an orphan drug by FDA for this indication. Efficacy of tisagenlecleucel for this use was evaluated in an open-label, multicenter, single-arm trial (JULIET) in patients ≥18 years of age with relapsed or refractory DLBCL who received 2 or more lines of chemotherapy or relapsed following autologous hematopoietic stem cell transplantation (HSCT). Treatment consisted of lymphodepleting chemotherapy (either fludarabine and cyclophosphamide or bendamustine) followed by a single IV infusion of tisagenlecleucel. The efficacy population consisted of a retrospectively identified subgroup of 68 patients who either had no bridging chemotherapy or had imaging that showed measurable disease after completion of bridging chemotherapy prior to tisagenlecleucel infusion. The overall response rate in this group was 50%; complete response rate was 32% and partial response rate was 18%. The median duration of response was not reached; however response rates were longer in patients who achieved complete response compared to patients with a best response of partial response.
Treatment of adults with relapsed or refractory (r/r) follicular lymphoma (FL) after two or more lines of systemic therapy. This indication is approved under accelerated approval based on response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s). Designated an orphan drug by FDA for this indication. Efficacy of tisagenlecleucel for this use was evaluated in an open-label, multicenter, single-arm trial (ELARA) in patients who had refractory or relapsed disease within 6 months after completion of 2 or more lines of systemic therapy. Treatment consisted of lymphodepleting chemotherapy (either fludarabine and cyclophosphamide or bendamustine) followed by a single IV infusion of tisagenlecleucel. A total of 90 patients with follicular lymphoma were included in the efficacy analysis. The overall response rate in this group was 86% and complete response rate was 68%. The median duration of response was not reached at a median follow-up of 9.1 months.
Tisagenlecleucel is an individualized cellular product prepared from autologous T cells obtained by leukapheresis. The patient's T-cells are sent to a laboratory where they are genetically modified to express chimeric antigen receptors (CAR), and then infused back into the patient.
CAR T-cell therapies can be associated with severe toxicities; the American Society of Clinical Oncology (ASCO) has published a guideline to provide guidance on the diagnosis, evaluation and management of such toxicities.
Related/similar drugs
prednisone, methotrexate, rituximab, cyclophosphamide, doxorubicin, Revlimid, Rituxan
Tisagenlecleucel Dosage and Administration
General
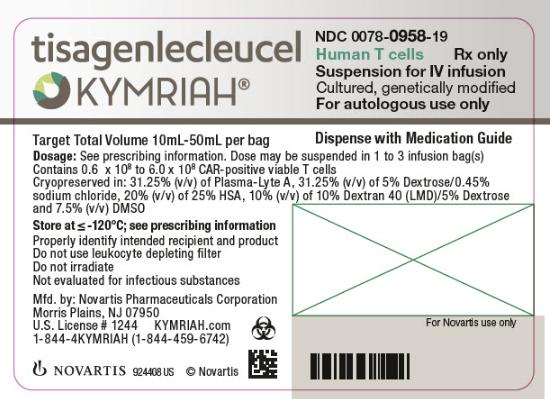
Tisagenlecleucel is available in the following dosage form(s) and strength(s):
-
Tisagenlecleucel is a cell suspension for IV infusion.
-
Pediatric and Young Adult B-cell ALL (up to 25 years of age): a single dose of tisagenlecleucel contains 0.2 to 5.0 x 106 CAR-positive viable T cells per kg of body weight for patients 50 kg or less, or 0.1 to 2.5 x 108 CAR-positive viable T cells for patients more than 50 kg, suspended in 1 to 3 patient-specific infusion bag(s) for IV infusion
-
Adult Relapsed or Refractory Diffuse Large B-cell Lymphoma and Follicular Lymphoma: a single dose of tisagenlecleucel contains 0.6 to 6.0 x 108 CAR-positive viable T cells suspended in 1 to 3 patient-specific infusion bag(s) for IV infusion.
-
See the certificate of analysis (CoA) for actual cell count. The volume in the infusion bag ranges from 10 mL to 50 mL.
Dosage
It is essential that the manufacturer's labeling be consulted for more detailed information on dosage and administration of this drug. Dosage summary:
Administer a lymphodepleting regimen if needed before infusion of tisagenlecleucel. Confirm the availability of tisagenlecleucel before starting lymphodepleting regimen. Lymphodepleting regimen differs based on indication. See Full Prescribing Information for additional information.
Do NOT use a leukodepleting filter.
Verify the patient’s identity prior to infusion. Check that the patient’s identity matches the patient identifiers on each infusion bag.
Premedicate with acetaminophen and an H1-antihistamine. Avoid prophylactic use of systemic corticosteroids as they may interfere with the activity of tisagenlecleucel.
Confirm availability of tocilizumab prior to infusion.
Pediatric Patients
Dosage Recommendations
For autologous use only. For IV use only.
-
Dosing of tisagenlecleucel is based on the number of chimeric antigen receptor (CAR)-positive viable T cells.
-
Dosage for Pediatric B-cell ALL: For patients 50 kg or less, administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight intravenously. For patients above 50 kg, administer 0.1 to 2.5 x 108 total CAR-positive viable T cells (non-weight based) intravenously.
Adults
Dosage Recommendations
For autologous use only. For IV use only.
-
Dosing of tisagenlecleucel is based on the number of chimeric antigen receptor (CAR)-positive viable T cells.
-
Young Adult B-cell ALL (up to 25 years of age): For patients 50 kg or less, administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight intravenously. For patients above 50 kg, administer 0.1 to 2.5 x 108 total CAR-positive viable T cells (non-weight based) intravenously.
-
Adult Relapsed or Refractory Diffuse Large B-cell Lymphoma and Follicular Lymphoma: Administer 0.6 to 6.0 x 108 CAR-positive viable T cells intravenously.
Cautions for Tisagenlecleucel
Contraindications
None.
Warnings/Precautions
Cytokine Release Syndrome (CRS)
CRS, including fatal or life-threatening reactions, occurred following treatment with tisagenlecleucel. CRS occurred in 61 (77%) of the 79 pediatric and young adult patients with relapsed or refractory (r/r) acute lymphoblastic leukemia (ALL) receiving tisagenlecleucel, including ≥ Grade 3 CRS (Penn grading system1) occurring in 48% of patients. The median times to onset and resolution of CRS were 3 days (range: 1-22; 1 patient with onset after Day 10) and 8 days (range: 1-36), respectively. Of the 61 patients with CRS, 31 (51%) received tocilizumab. Ten (16%) patients received two doses of tocilizumab and 3 (5%) patients received three doses of tocilizumab; 17 (28%) patients received addition of corticosteroids (e.g., methylprednisolone).
CRS occurred in 85 (74%) of the 115 adult patients with r/r diffuse large B-cell lymphoma (DLBCL) receiving tisagenlecleucel, including ≥ Grade 3 CRS (Penn grading system1) occurring in 23% of patients. The median times to onset and resolution of CRS were 3 days (range: 1-51; 1 patient with onset after Day 10) and 7 days (range: 2-30), respectively. Of the 85 patients with CRS, 19 (22%) received systemic tocilizumab or corticosteroids. Seven (8%) patients received a single dose of tocilizumab and 11 (13%) patients received two doses of tocilizumab; 11 (13%) patients received corticosteroids in addition to tocilizumab. One patient received corticosteroids for CRS without concomitant tocilizumab, and two patients received corticosteroids for persistent neurotoxicity after resolution of CRS.
CRS occurred in 51 (53%) of the 97 adult patients with r/r follicular lymphoma (FL) receiving tisagenlecleucel; all were Grade 1 or 2 CRS (Lee grading system2). The median times to onset and resolution of CRS were 4 days (range: 1-14) and 4 days (range: 1-13), respectively. Of the 51 patients with CRS, 15 (29%) received systemic anticytokine treatment with tocilizumab. Three (6%) patients required 3 dosages of tocilizumab, 4 (8%) patients required 2 dosages and 8 (16%) patients required single dose of tocilizumab. Two (4%) patients received corticosteroids in addition to tocilizumab.
Five deaths occurred within 30 days of tisagenlecleucel infusion. One patient with r/r ALL died with CRS and progressive leukemia, and one patient had resolving CRS with abdominal compartment syndrome, coagulopathy, and renal failure when an intracranial hemorrhage occurred. Of the 3 r/r DLBCL patients who died within 30 days of infusion, all had CRS in the setting of stable to progressive underlying disease, one of whom developed bowel necrosis.
Among patients with CRS, key manifestations include fever (93% in r/r ALL; 85% in r/r DLBCL; 92% in r/r FL), hypotension (69% in r/r ALL; 45% in r/r DLBCL; 40% in r/r FL), hypoxia (57% in r/r ALL; 35% in r/r DLBCL; 19% in r/r FL), and tachycardia (26% in r/r ALL; 13% in r/r DLBCL; 2% in r/r FL). CRS may be associated with hepatic, renal, and cardiac dysfunction, and coagulopathy.
Delay the infusion of tisagenlecleucel after lymphodepleting chemotherapy if the patient has unresolved serious adverse reactions from preceding chemotherapies (including pulmonary toxicity, cardiac toxicity, or hypotension), active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden.
Risk factors for severe CRS in the pediatric and young adult r/r B-cell ALL population are high pre-infusion tumor burden (greater than 50% blasts in bone marrow), uncontrolled or accelerating tumor burden following lymphodepleting chemotherapy, active infections, and/or inflammatory processes.
Ensure that a minimum of two doses of tocilizumab are available on site prior to infusion of tisagenlecleucel.
Monitor patients 2-3 times during the first week following tisagenlecleucel infusion at the REMS-certified healthcare facility for signs and symptoms of CRS. Monitor patients for signs or symptoms of CRS for at least 4 weeks after treatment with tisagenlecleucel. At the first sign of CRS, immediately evaluate patient for hospitalization and institute treatment with supportive care, tocilizumab and/or corticosteroids as indicated.
Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time.
Neurological Toxicities
Neurological toxicities, including severe or life-threatening reactions, occurred following treatment with tisagenlecleucel. Neurologic toxicities occurred in 56 (71%) of the 79 patients with r/r ALL, including ≥ Grade 3 in 22%. The median times to the first event and duration were 6 days from infusion (range: 1-301) and 7 days, respectively.
Neurologic toxicities occurred in 69 (60%) of the 115 patients with r/r DLBCL, including ≥ Grade 3 in 19%. The median times to the first event and duration were 5 days (range: 1-368) and 17 days, respectively.
Neurologic toxicities occurred in 42 (43%) of the 97 patients with r/r FL, including ≥ Grade 3 in 6%. The median times to the first event and duration were 8 days (range: 1-345) and 5 days, respectively.
Among patients who had a neurological toxicity, 84% occurred within 8 weeks following tisagenlecleucel infusion. Resolution occurred within 3 weeks in 71% of patients with r/r ALL, 50% of patients with r/r DLBCL, and 74% of patients with r/r FL. Encephalopathy lasting up to 70 days was noted.
The onset of neurological toxicity can be concurrent with CRS, following resolution of CRS or in the absence of CRS.
The most common neurological toxicities observed with tisagenlecleucel include headache (35% in r/r ALL; 21% in r/r DLBCL; 25% in r/r FL), encephalopathy (30% in r/r ALL; 16% in r/r DLBCL; 3% in r/r FL), delirium (19% in r/r ALL; 5% in r/r DLBCL; 1% in r/r FL), anxiety (16% in r/r ALL; 10% in r/r DLBCL; 2% in r/r FL), sleep disorders (11% in r/r ALL; 10% in r/r DLBCL; 6% in r/r FL), dizziness (5% in r/r ALL; 12% in r/r DLBCL; 8% of r/r FL), tremor (8% in r/r ALL; 6% r/r DLBCL; 3% of r/r FL), and peripheral neuropathy (4% in r/r ALL; 12% in r/r DLBCL; 7% in r/r FL). Other manifestations included seizures and aphasia.
Monitor patients 2-3 times during the first week following tisagenlecleucel infusion at the REMS-certified healthcare facility for signs and symptoms of neurologic toxicities. Rule out other causes of neurological symptoms. Monitor patients for signs or symptoms of neurologic toxicities for at least 4 weeks after infusion and treat promptly. Neurologic toxicity should be managed with supportive care and/or corticosteroids as needed.
Counsel patients to seek immediate medical attention should signs or symptoms of neurologic toxicity occur at any time.
REMS
Because of the risk of CRS and neurological toxicities, tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Kymriah REMS. Healthcare facilities that dispense and administer tisagenlecleucel must be enrolled and comply with the REMS requirements. Certified healthcare facilities must have on-site, immediate access to tocilizumab, and ensure that a minimum of two doses of tocilizumab are available for each patient for administration within 2 hours after tisagenlecleucel infusion, if needed for treatment of CRS. Certified healthcare facilities must ensure that healthcare providers who prescribe, dispense or administer tisagenlecleucel are trained about the management of CRS and neurological toxicities. Further information is available at www.kymriah-rems.com or 1-844-4kymriah.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS)
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS), which can be life-threatening or fatal, has occurred following treatment with tisagenlecleucel. HLH was reported in 6% (5/79) of patients with r/r ALL (time to onset ranged from 3 to 18 days) and 2% (2/115) of patients with r/r DLBCL (times to onset were Day 7 and Day 10); all HLH events occurred during ongoing CRS and resolved. One patient (1%) with r/r FL developed HLH > 1 year after receiving tisagenlecleucel with a fatal outcome. The patient did not have CRS during or immediately preceding HLH. Treatment of HLH should be administered as per institutional standards.
Hypersensitivity Reactions
Allergic reactions may occur with infusion of tisagenlecleucel. Serious hypersensitivity reactions, including anaphylaxis, may be due to the DMSO or dextran 40 in tisagenlecleucel. Observe patients for hypersensitivity reactions during the infusion.
Serious Infections
Infections, including life-threatening or fatal infections, occurred following treatment with tisagenlecleucel. Infections occurred in 57 (72%) of the 79 patients with r/r ALL; 38 patients (48%) experienced ≥ Grade 3 infections, including fatal infections in 2 patients (3%).
Infections occurred in 67 (58%) of the 115 patients with r/r DLBCL; 38 patients (33%) experienced ≥ Grade 3 infections, including fatal infection in 1 patient (1%).
Infections occurred in 50 (52%) of the 97 patients with r/r FL; 20 patients (21%) experienced ≥ Grade 3 infections, including fatal infection in 1 patient (1%).
Prior to tisagenlecleucel infusion, infection prophylaxis should follow local guidelines. Patients with active uncontrolled infection should not start tisagenlecleucel treatment until the infection is resolved. Monitor patients for signs and symptoms of infection after treatment with tisagenlecleucel and treat appropriately.
Febrile neutropenia (≥ Grade 3) was also observed in 34% of patients with r/r ALL, 17% of patients with r/r DLBCL, and 13% of patients with r/r FL after tisagenlecleucel infusion and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage with broad spectrum antibiotics, fluids and other supportive care as medically indicated.
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure and death, can occur in patients treated with drugs directed against B cells.
There is no experience with manufacturing tisagenlecleucel for patients with a positive test for HIV or with active HBV or active HCV. Perform screening for HBV, HCV, and HIV in accordance with clinical guidelines before collection of cells for manufacturing.
Prolonged Cytopenias
Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and tisagenlecleucel infusion.
In the ELIANA study (Study 1), ≥ Grade 3 cytopenias not resolved by Day 28 following tisagenlecleucel treatment included neutropenia (40%), and thrombocytopenia (27%) among 52 responding patients. At 56 days following tisagenlecleucel, 17% and 12% of responding patients had ≥ Grade 3 neutropenia or thrombocytopenia, respectively.
In the JULIET study (Study 2), ≥ Grade 3 cytopenias not resolved by Day 28 following tisagenlecleucel treatment included thrombocytopenia (39%) and neutropenia (25%) among 115 treated patients.
In the ELARA study (Study 3), ≥ Grade 3 cytopenias not resolved by Day 28 following tisagenlecleucel treatment included thrombocytopenia (17%) and neutropenia (16%) among 97 treated patients.
Prolonged neutropenia has been associated with increased risk of infection. Myeloid growth factors, particularly GM-CSF, are not recommended during the first 3 weeks after tisagenlecleucel infusion or until CRS has resolved.
Hypogammaglobulinemia
Hypogammaglobulinemia and agammaglobulinemia related to B-cell aplasia can occur in patients after tisagenlecleucel infusion.
Hypogammaglobulinemia was reported in 53% of patients treated with tisagenlecleucel for r/r ALL, 17% of patients with r/r DLBCL, and 18% of patients with r/r FL.
Monitor immunoglobulin levels after treatment with tisagenlecleucel and manage using infection precautions, antibiotic prophylaxis, and immunoglobulin replacement standard guidelines.
The safety of immunization with live vaccines during or following tisagenlecleucel treatment has not been studied. Vaccination with live vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during tisagenlecleucel treatment, and until immune recovery following treatment with tisagenlecleucel.
Pregnant women who have received tisagenlecleucel may have hypogammaglobulinemia. Assess immunoglobulin levels in newborns of mothers treated with tisagenlecleucel.
Secondary Malignancies
Patients treated with tisagenlecleucel may develop secondary malignancies or recurrence of their cancer. Monitor life-long for secondary malignancies. In the event that a secondary malignancy occurs, contact Novartis Pharmaceuticals Corporation at 1-844-4KYMRIAH to obtain instructions on patient samples to collect for testing.
Effects on Ability to Drive and Use Machines
Due to the potential for neurological events, including altered mental status or seizures, patients receiving tisagenlecleucel are at risk for altered or decreased consciousness or coordination in the 8 weeks following tisagenlecleucel infusion. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, during this initial period.
Specific Populations
Pregnancy
There are no available data with tisagenlecleucel use in pregnant women. No animal reproductive and developmental toxicity studies have been conducted with tisagenlecleucel to assess whether it can cause fetal harm when administered to a pregnant woman. It is not known if tisagenlecleucel has the potential to be transferred to the fetus. Based on the mechanism of action, if the transduced cells cross the placenta, they may cause fetal toxicity, including B-cell lymphocytopenia. Therefore, tisagenlecleucel is not recommended for women who are pregnant, and pregnancy after tisagenlecleucel administration should be discussed with the treating physician. Report pregnancies to Novartis Pharmaceuticals Corporation at 1-888-669-6682.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Lactation
There is no information regarding the presence of tisagenlecleucel in human milk, the effect on the breastfed infant, and the effects on milk production. A risk to the breastfed infant cannot be excluded. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for tisagenlecleucel and any potential adverse effects on the breastfed infant from tisagenlecleucel or from the underlying maternal condition.
Females and Males of Reproductive Potential
Pregnancy status of females with reproductive potential should be verified. Sexually-active females of reproductive potential should have a pregnancy test prior to starting treatment with tisagenlecleucel.
See the prescribing information for fludarabine and cyclophosphamide for information on the need for effective contraception in patients who receive the lymphodepleting chemotherapy.
There are insufficient exposure data to provide a recommendation concerning duration of contraception following treatment with tisagenlecleucel.
There are no data on the effect of tisagenlecleucel on male and female fertility.
Pediatric Use
The safety and efficacy of tisagenlecleucel have been established in pediatric patients with r/r B-cell ALL. Use of tisagenlecleucel is supported by a single-arm trial that included 61 pediatric patients with r/r B-cell precursor ALL in the following age groups: 40 children (ages 2 years to less than 12 years) and 21 adolescents (ages 12 years to less than 17 years). No differences in efficacy or safety were observed between the different age subgroups or in comparison to the young adults in the trial.
The safety and efficacy of tisagenlecleucel in pediatric patients with r/r DLBCL and r/r FL have not been established.
Geriatric Use
The safety and effectiveness of tisagenlecleucel have not been established in geriatric patients with r/r B-cell ALL. Clinical studies of tisagenlecleucel did not include sufficient numbers of patients 65 years of age and older to determine whether they respond differently from younger subjects.
Common Adverse Effects
Pediatric and Young Adult B-cell ALL (up to 25 years of age): The most common adverse reactions (incidence greater than 20%) are cytokine release syndrome, infections-pathogen unspecified, hypogammaglobulinemia, fever, decreased appetite, viral infectious disorders, headache, febrile neutropenia, hemorrhage, musculoskeletal pain, vomiting, encephalopathy, diarrhea, hypotension, cough, nausea, bacterial infectious disorders, pain, hypoxia, tachycardia, edema, fatigue, and acute kidney injury.
Adult Relapsed or Refractory Diffuse Large B-cell Lymphoma: The most common adverse reactions (incidence greater than 20%) are CRS, infections-pathogen unspecified, fever, diarrhea, nausea, fatigue, hypotension, edema, hemorrhage, dyspnea, and headache.
Adult Relapsed or Refractory Follicular Lymphoma: The most common adverse reactions (incidence greater than 20%) are cytokine release syndrome, infections-pathogens unspecified, fatigue, musculoskeletal pain, headache, and diarrhea.
Drug Interactions
Specific Drugs
It is essential that the manufacturer's labeling be consulted for more detailed information on interactions with this drug, including possible dosage adjustments. Interaction highlights:
HIV and the lentivirus used to make tisagenlecleucel have limited, short spans of identical genetic material (RNA). Therefore, some commercial HIV nucleic acid tests (NATs) may yield false-positive results in patients who have received tisagenlecleucel.
Actions
Mechanism of Action
Tisagenlecleucel is a chimeric antigen receptor (CAR)-positive T-cell therapy consisting of genetically modified autologous T cells that bind to CD19. The CAR T-cell immunotherapy involves reprogramming a patient’s own T cells with a transgene encoding a CAR to identify and eliminate CD19-expressing malignant and normal cells. The CAR is comprised of a murine single-chain antibody fragment which recognizes CD19 and is fused to intracellular signaling domains from 4-1BB (CD137) and CD3 zeta. The CD3 zeta component is critical for initiating T cell activation and antitumor activity, while 4-1BB enhances the expansion and persistence of tisagenlecleucel. Upon binding to CD19-expressing cells, the CAR transmits a signal to promote T cell expansion, activation, target cell elimination, and persistence of the tisagenlecleucel cells.
Advice to Patients
-
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
-
Ensure that patients understand the risk of manufacturing failure. This has been reported in up to 9% of manufacturing attempts. In case of a manufacturing failure, a second manufacturing of tisagenlecleucel may be attempted. In addition, while the patient awaits the product, additional chemotherapy (not the lymphodepletion) may be necessary and may increase the risk of adverse events during the pre-infusion period.
-
Advise patients to report signs and symptoms of Cytokine Release Syndrome (CRS) to their healthcare professional. Signs or symptoms associated with CRS include high fever, difficulty breathing, chills/shaking chills, severe nausea, severe vomiting, severe diarrhea, severe muscle pain, severe joint pain, very low blood pressure, or dizziness/lightheadedness.
-
Advise patients to report signs and symptoms of neurologic tioxicity (e.g., altered or decreased consciousness, delirium, confusion, agitation, seizures, difficulty speaking and understanding, loss of balance) to their healthcare professional.
-
Advise patients of the risk of Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS). Inform patients that the presenting signs and symptoms are similar to those of CRS and infections.
-
Advise patients that tisagenlecleucel may cause serious infections and that they will be screened for HBV, HCV, and HIV before collection of cells.
-
Advise patients of the risk of hypogammaglobulinemia and that they may need to receive immunoglobulin replacement for an indefinite amount of time following treatment with tisagenlecleucel. Patients should tell their physician about their treatment with tisagenlecleucel before receiving a live vaccine.
-
Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, for at least 8 weeks after treatment.
-
Advise patients that they may exhibit signs or symptoms associated with bone marrow suppression (i.e., neutropenia, thrombocytopenia and anemia) for several weeks following lymphodepleting chemotherapy and tisagenlecleucel.
-
Instruct patients to contact Novartis Pharmaceuticals Corporation at 1-844-4KYMRIAH if they get secondary malignancies
Additional Information
AHFSfirstRelease™. For additional information until a more detailed monograph is developed and published, the manufacturer's labeling should be consulted. It is essential that the manufacturer's labeling be consulted for more detailed information on usual uses, dosage and administration, cautions, precautions, contraindications, potential drug interactions, laboratory test interferences, and acute toxicity.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Suspension, for IV infusion |
1.2 x 106 to 2.5 x 108 CAR-positive viable T cells |
Kymriah (supplied in 1 to 3 bags containing a frozen suspension of genetically modified autologous T cells in infusion bag(s) labeled for specific recipient) |
Novartis Pharmaceuticals Corporation |
|
0.6 x 108 to 6.0 x 108 CAR-positive viable T cells |
Kymriah (supplied in 1 to 3 bags containing a frozen suspension of genetically modified autologous T cells in infusion bag(s) labeled for specific recipient) |
Novartis Pharmaceuticals Corporation |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions September 29, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about tisagenlecleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- En español