Esomeprazole (Monograph)
Brand names: NexIUM, Vimovo (combination)
Drug class: Proton-pump Inhibitors
VA class: GA900
Chemical name: 5-Methoxy-2-[(S)[(4-methoxy-3,5-dimethyl-2-pyridinyl)methyl]sulfinyl]-1H-benzimidazole magnesium salt trihydrate
Molecular formula: C34H36MgN6O6S2•3H2OC17H18N3O3S•Na
CAS number: 217087-09-7
Introduction
Acid- or proton-pump inhibitor; gastric antisecretory agent.1 3 5 19 34 S-isomer of omeprazole.1 5 9 34
Uses for Esomeprazole
Gastroesophageal Reflux (GERD)
Short-term treatment of symptomatic GERD (e.g., heartburn) in patients without erosive esophagitis.1
Short-term treatment of erosive esophagitis (diagnostically confirmed) in patients with GERD.1 Short-term treatment of erosive esophagitis due to acid-mediated GERD in infants.1
Maintain healing, symptom resolution, and decrease recurrence of erosive esophagitis.1
IV as short-term alternative to oral therapy in patients with erosive esophagitis who are unable to take the drug orally; safety and efficacy not established beyond 10 days.34
Duodenal Ulcer
Treatment of Helicobacter pylori infection and duodenal ulcer disease (active duodenal ulcer or history of duodenal ulcer in the past 5 years).1 Used in conjunction with amoxicillin and clarithromycin (triple therapy).1
NSAIA-associated Ulcers
Reduction in the occurrence of gastric ulcers associated with chronic NSAIA therapy in patients at risk (i.e., ≥60 years of age and/or history of gastric ulcer).1 33 342 Effect on occurrence of duodenal ulcers not established.1 33
Crohn’s Disease-associated Ulcers
Some evidence for use of proton-pump inhibitors (e.g., omeprazole) for gastric acid suppressive therapy as an adjunct in the management of upper GI Crohn’s disease† [off-label], including esophageal, gastroduodenal, and jejunoileal disease.22 23 24 25 26 27 28
Related/similar drugs
amoxicillin, omeprazole, famotidine, pantoprazole, metronidazole, Protonix, sucralfate
Esomeprazole Dosage and Administration
Administration
Oral Administration
Administer esomeprazole capsules and oral suspension orally at least 1 hour before a meal.1 Administer esomeprazole/naproxen fixed-combination tablets at least 30 minutes before a meal.342 (See Food under Pharmacokinetics.)
Antacids may be used concomitantly as needed for pain relief.1
Capsules
Swallow capsules intact; do not chew or crush.1
Alternatively, open capsule and mix contents with 1 tablespoon applesauce; swallow immediately without chewing.1 Applesauce should not be hot and should be soft enough to swallow without chewing.1
Powder for Oral Suspension
Mix contents of 2.5- or 5-mg packet with 5 mL of water.1
Mix contents of 10-, 20-, or 40-mg packet with 15 mL of water.1
If a single dose requires 2 packets, reconstitute oral suspension with twice the water needed for 1 packet.1
After mixing suspension with appropriate amount of water, allow mixture to thicken for 2–3 minutes.1 Stir mixture and consume within 30 minutes of preparation.1 If any drug mixture remains in container after ingestion, mix with additional water and ingest immediately.1
NG Tube
May administer suspension prepared from opened capsules through NG tube; may administer suspension prepared from powder for oral suspension through NG tube or gastric tube (6 French or larger).1
Capsules: Open capsule, empty intact granules into 60-mL catheter-tipped syringe, and mix with 50 mL of water.1 Replace plunger and shake well for 15 seconds.1 Hold syringe with tip upright and check tip for remaining granules.1 Administer immediately through NG tube; flush with additional water.1 Do not administer if pellets have dissolved or disintegrated.1
Powder for oral suspension: Mix contents of 2.5- or 5-mg packet with 5 mL of water and contents of 10-, 20-, or 40-mg packet with 15 mL of water in a catheter-tipped syringe; shake immediately, then allow mixture to thicken for 2–3 minutes.1 Shake syringe and administer through NG or gastric tube (6 French or larger) within 30 minutes of preparation.1 Refill syringe with additional water (5 or 15 mL, respectively) and flush NG or gastric tube.1
Esomeprazole/Naproxen Fixed-combination Tablets
Swallow tablets whole with liquid; do not split, chew, crush, or dissolve tablets.342
IV Administration
For solution compatibility information, see Compatibility under Stability.
Administer by slow direct IV injection or by IV infusion.34
Flush the IV line with 0.9% sodium chloride, lactated Ringer’s, or 5% dextrose injection before and after administration.34
Do not administer with any other drugs or diluents because of potential incompatibilities.34
Reconstitution
For direct IV injection in adults, reconstitute vial containing 20 or 40 mg of esomeprazole with 5 mL of 0.9% sodium chloride injection.34
For IV infusion in adults, reconstitute vial containing 20 or 40 mg of esomeprazole with 5 mL of 5% dextrose, 0.9% sodium chloride, or lactated Ringer’s injection.34 Dilute reconstituted solution prior to infusion.34
For IV infusion in pediatric patients 1 month to 17 years of age, reconstitute vial containing 20 or 40 mg of esomeprazole with 5 mL of 0.9% sodium chloride injection to provide a solution containing 4 or 8 mg/mL, respectively.34 Dilute reconstituted solution prior to infusion.34
Dilution
For IV infusion in adults, dilute the reconstituted solution to a final volume of 50 mL with a compatible IV solution (see Compatibility under Stability).34
For IV infusion in pediatric patients 1 month to 17 years of age, dilute the reconstituted 4- or 8-mg/mL solution to a final volume of 50 mL with 0.9% sodium chloride injection to yield a final concentration of 0.4 or 0.8 mg/mL, respectively.34 Withdraw the appropriate dose from the diluted solution.34
Rate of Administration
IV injection in adults: Administer reconstituted solution by slow (over ≥3 minutes) direct IV injection.34
IV infusion in adults and pediatric patients: Administer diluted solution by IV infusion over 10–30 minutes.34
Dosage
Available as esomeprazole magnesium and esomeprazole sodium; dosage expressed in terms of esomeprazole.1 34
Pediatric Patients
GERD
GERD Without Erosive Esophagitis
OralChildren 1–11 years of age: 10 mg once daily for up to 8 weeks.1
Adolescents 12–17 years of age: 20 or 40 mg once daily for up to 8 weeks.1
Treatment of Erosive Esophagitis
Oral|
Age |
Body Weight |
Esomeprazole Dosage |
|---|---|---|
|
1 month to <1 year of age |
3–5 kg |
2.5 mg once daily for up to 6 weeks |
|
>5 to 7.5 kg |
5 mg once daily for up to 6 weeks |
|
|
>7.5 to 12 kg |
10 mg once daily for up to 6 weeks |
|
|
1–11 years of age |
<20 kg |
10 mg once daily for up to 8 weeks |
|
≥20 kg |
10 or 20 mg once daily for up to 8 weeks |
Infants 1 month to <1 year of age: 0.5 mg/kg once daily.34 48
Children and adolescents 1–17 years of age: 10 mg once daily in those weighing <55 kg; 20 mg once daily in those weighing ≥55 kg.34 48
Discontinue IV administration as soon as patient can take the drug orally.34
Adults
GERD
GERD Without Erosive Esophagitis
Oral20 mg once daily for 4 weeks; may give an additional 4 weeks of therapy.1 Chronic proton-pump inhibitor therapy may be appropriate.21
Treatment of Erosive Esophagitis
Oral20 or 40 mg once daily for 4–8 weeks;1 may give an additional 4–8 weeks of therapy.1
IV20 or 40 mg once daily.34 Safety and efficacy not established beyond 10 days; discontinue IV administration as soon as patient can take the drug orally.34
Maintenance of Healing of Erosive Esophagitis
Oral20 mg once daily; not studied >6 months.1
Duodenal Ulcer
Helicobacter pylori Infection and Duodenal Ulcer
OralTriple therapy: 40 mg once daily for 10 days in conjunction with amoxicillin and clarithromycin.1
NSAIA-associated Ulcers
Prevention of Gastric Ulcers
Oral20 or 40 mg once daily; not studied >6 months.1
Esomeprazole/naproxen fixed combination: Esomeprazole 20 mg (with naproxen 375 or 500 mg) twice daily.342 Do not use fixed combination if esomeprazole dosage requirement is <40 mg daily.342
Prescribing Limits
Pediatric Patients
GERD
GERD Without Erosive Esophagitis
OralChildren 1–11 years of age: Dosages >1 mg/kg daily not studied.1
Treatment of Erosive Esophagitis
OralInfants 1 month to <1 year of age: Dosages >1.33 mg/kg daily not studied.1
Children 1–11 years of age: Dosages >1 mg/kg daily not studied.1
Special Populations
Hepatic Impairment
Oral or IV dosage should not exceed 20 mg once daily in patients with severe (Child-Pugh class C) hepatic impairment.1 34 342 No dosage adjustment required for mild or moderate (Child-Pugh class A or B, respectively) hepatic impairment.1 34
Esomeprazole/naproxen fixed combination not recommended in patients with severe hepatic impairment.342
Renal Impairment
Esomeprazole/naproxen fixed combination not recommended in patients with Clcr <30 mL/minute.342
Cautions for Esomeprazole
Contraindications
-
Known hypersensitivity to esomeprazole, any ingredient in the formulation, or other substituted benzimidazoles (e.g., lansoprazole, omeprazole, pantoprazole, rabeprazole).1 34
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., angioedema, anaphylactic shock) reported.1 34
Gastric Malignancy
Response to esomeprazole does not preclude presence of occult gastric neoplasm.1 34
Atrophic Gastritis
Atrophic gastritis reported occasionally with long-term omeprazole use.1 34
Clostridium difficile Infection
Proton-pump inhibitors associated with possible increased (1.4–2.75 times) risk of Clostridium difficile infection, including C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis).335 336 339 340 Many patients also had other risk factors for CDAD.335 May be severe; colectomy and, rarely, death reported.335
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient's clinical condition.335
Consider CDAD if persistent diarrhea develops and manage accordingly; initiate supportive therapy (e.g., fluid and electrolyte management), anti-infective therapy directed against C. difficile (e.g., metronidazole, vancomycin), and surgical evaluation as clinically indicated.335 336
Bone Fracture
Several observational studies suggest that use of proton-pump inhibitors, particularly in high dosages (i.e., multiple daily doses) and/or for prolonged periods of time (i.e., ≥1 year), may be associated with increased risk of osteoporosis-related fractures of the hip, wrist, or spine.1 34 35 300 301 302 303 304 305 Magnitude of risk is unclear;35 300 301 302 303 304 305 310 causality not established.305 FDA is continuing to evaluate this safety concern.305
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient’s clinical condition.1 34 35 301 303 305 307
Individuals at risk for osteoporosis-related fractures should receive an adequate intake of calcium and vitamin D; assess and manage these patients’ bone health according to current standards of care.1 34 35 303 305 307
Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, reported rarely in patients receiving long-term therapy (≥3 months or, in most cases, >1 year) with proton-pump inhibitors, including esomeprazole.1 34 317 318 319 320 321 322 323 324 325 326 327 328 329 330 Serious adverse effects include tetany, seizures, tremors, carpopedal spasm, arrhythmias (e.g., atrial fibrillation, supraventricular tachycardia), and abnormal QT interval.1 34 318 319 321 322 323 325 327 328 329 Paresthesia, muscle weakness, muscle cramps, lethargy, fatigue, and unsteadiness may occur.319 320 321 325 330 Most patients required magnesium replacement and discontinuance of the proton-pump inhibitor.1 34 317 319 321 322 323 324 325 326 327 330 Hypomagnesemia resolved within 1 week (median) following discontinuance and recurred within 2 weeks (median) of rechallenge.327
In patients expected to receive long-term proton-pump inhibitor therapy or in patients currently receiving digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), consider measuring serum magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter.1 34 319 326 327 328 330
Cardiovascular Effects
Preliminary safety data from 2 long-term clinical trials comparing esomeprazole or omeprazole with antireflux surgery in patients with severe GERD raised concerns about a potential increased risk of cardiac events (e.g., MI, heart failure, sudden death) in patients receiving these drugs.36 37 38 After reviewing data from these and other studies, FDA has concluded that long-term use of these drugs is not likely to be associated with an increased risk of such cardiac events.36 37 38 FDA recommends that clinicians continue to prescribe and patients continue to use these drugs in the manner described in the manufacturers’ labelings.36 37 38
Respiratory Effects
Administration of proton-pump inhibitors has been associated with an increased risk for developing certain infections (e.g., community-acquired pneumonia).29 30
Use of Fixed Combinations
When used in fixed combination with naproxen, consider the cautions, precautions, and contraindications associated with naproxen.342
Specific Populations
Pregnancy
Lactation
Not known whether esomeprazole is distributed into milk, but omeprazole is distributed into milk.1 34 Discontinue nursing or the drug.1 34
Pediatric Use
Safety and efficacy of oral esomeprazole for short-term (4–8 weeks) treatment of GERD established in pediatric patients 1–17 years of age.1 Adverse effects and pharmacokinetics in children and adolescents similar to those reported in adults.1
Safety and efficacy of oral esomeprazole for short-term (up to 6 weeks) treatment of erosive esophagitis due to acid-mediated GERD established in infants 1 month to <1 year of age.1 Oral esomeprazole was not more effective than placebo in a randomized, controlled, treatment-withdrawal study in infants 1–11 months of age with symptomatic GERD.1 Common adverse effects include irritability and vomiting.1
Efficacy of oral esomeprazole not established in infants <1 month of age.1
Safety and efficacy of IV esomeprazole for short-term treatment of GERD with erosive esophagitis established in pediatric patients 1 month to 17 years of age.34 Adverse effects consistent with the drug's known safety profile.34
Safety and efficacy of IV esomeprazole in neonates <1 month of age not established.34
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.1 34
Hepatic Impairment
Use with caution in patients with severe hepatic impairment.1 20 (See Hepatic Impairment under Dosage and Administration.)
Common Adverse Effects
Oral: Headache, diarrhea, nausea, flatulence, abdominal pain, constipation, dry mouth.1 19
IV: Similar adverse effects as oral esomeprazole; also injection site reaction, dizziness/vertigo, pruritus.34
Drug Interactions
Extensively metabolized by CYP isoenzymes, principally CYP2C19; also to lesser extent by CYP3A4.1 19 34 May inhibit CYP2C19; unlikely to inhibit CYP3A4, 1A2, 2A6, 2C9, 2D6, or 2E1.1 34
Drugs Metabolized by Hepatic Microsomal Enzymes
Potential to inhibit metabolism of drugs metabolized by CYP2C19.1 34 Interaction unlikely with drugs metabolized by other CYP isoenzymes.1 34
Drugs Affecting Hepatic Microsomal Enzymes
Combined inhibitors of CYP2C19 and CYP3A4: Potential pharmacokinetic interaction (increased esomeprazole exposure); esomeprazole dosage adjustment usually not required but may be considered in patients receiving high dosages (up to 240 mg daily), such as those with Zollinger-Ellison syndrome.1 34
Inducers of CYP2C19 and/or CYP3A4: Potential pharmacokinetic interaction (decreased esomeprazole concentrations).1 34
Drugs that Cause Hypomagnesemia
Potential pharmacologic interaction (possible increased risk of hypomagnesemia).327 Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter.1 34 327 (See Hypomagnesemia under Cautions.)
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Amoxicillin |
||
|
Atazanavir |
Possible altered oral absorption of atazanavir, resulting in decreased plasma atazanavir concentrations; possible loss of virologic response and development of drug resistance1 31 34 |
Manufacturer of esomeprazole states that concomitant administration with atazanavir is not recommended1 34 Antiretroviral treatment-naive patients: If a proton-pump inhibitor is used concomitantly with atazanavir, administer ritonavir-boosted atazanavir (atazanavir 300 mg and ritonavir 100 mg once daily with food); administer the proton-pump inhibitor approximately 12 hours before ritonavir-boosted atazanavir31 32 For treatment-naive patients, dosage of proton-pump inhibitor should not exceed omeprazole 20 mg daily (or equivalent)31 32 Antiretroviral treatment-experienced patients: Concomitant use of proton-pump inhibitors with atazanavir not recommended31 32 |
|
Cilostazol |
Possible increased concentrations of cilostazol and its active metabolite1 34 |
Consider reducing cilostazol dosage (from 100 mg twice daily to 50 mg twice daily)1 34 |
|
Clarithromycin |
Increased plasma concentrations of esomeprazole and 14-hydroxyclarithromycin 1 |
|
|
Clopidogrel |
Esomeprazole (or omeprazole) reduces exposure to clopidogrel's active metabolite and decreases platelet inhibitory effects;44 224 225 228 232 233 236 350 additional data needed to fully elucidate potential clinical consequences (e.g., increased cardiovascular events)40 41 42 44 45 224 225 228 229 230 235 236 237 238 240 311 Dexlansoprazole, lansoprazole, or pantoprazole had less effect on clopidogrel's antiplatelet activity than did omeprazole or esomeprazole224 350 351 |
Avoid concomitant use of esomeprazole (or omeprazole) and clopidogrel224 Assess risks and benefits of concomitant proton-pump inhibitor and clopidogrel use in individual patients312 313 314 315 316 American College of Cardiology Foundation/American College of Gastroenterology/American Heart Association (ACCF/ACG/AHA) states that GI bleeding risk reduction with concomitant proton-pump inhibitor in patients with risk factors for GI bleeding (e.g., advanced age; concomitant use of warfarin, corticosteroids, or NSAIAs; H. pylori infection) may outweigh potential reduction in cardiovascular efficacy of antiplatelet treatment associated with a drug-drug interaction.311 In patients without such risk factors, ACCF/ACG/AHA states that risk/benefit balance may favor use of antiplatelet therapy without a proton-pump inhibitor.311 If concomitant therapy with a proton-pump inhibitor and clopidogrel is deemed necessary, consider using an agent with little or no CYP2C19-inhibitory activity;44 45 46 224 230 350 alternatively, consider using a histamine H2-receptor antagonist (ranitidine, famotidine, nizatidine)44 45 230 but not cimetidine (also a potent CYP2C19 inhibitor)232 233 |
|
Diazepam |
Decreased diazepam metabolism and increased plasma concentrations1 34 |
|
|
Digoxin |
Hypomagnesemia (e.g., resulting from long-term use of proton-pump inhibitors) sensitizes the myocardium to digoxin and, thus, may increase risk of digoxin-induced cardiotoxic effects327 331 See table entry for gastric pH-dependent drugs |
Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter1 327 |
|
Diuretics (i.e., loop or thiazide diuretics) |
Possible increased risk of hypomagnesemia327 |
Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter1 327 |
|
Fosamprenavir |
Fosamprenavir: Increased esomeprazole AUC; no substantial effect on concentrations of amprenavir (active metabolite of fosamprenavir)345 Ritonavir-boosted fosamprenavir: No substantial effect on amprenavir or esomeprazole concentrations345 |
Fosamprenavir (with or without ritonavir): No dosage adjustment required32 345 |
|
Gastric pH-dependent drugs (e.g., atazanavir, digoxin, erlotinib, iron salts, ketoconazole) |
Atazanavir, erlotinib, iron salts, ketoconazole: Possible decreased absorption1 34 |
Digoxin: May need to monitor for manifestations of digoxin toxicity1 34 |
|
Lopinavir |
Lopinavir/ritonavir: Omeprazole had no clinically important effect on lopinavir plasma concentrations or AUC32 344 |
No dosage adjustment required when proton-pump inhibitors used with lopinavir/ritonavir32 |
|
Methotrexate |
Possible delayed clearance and increased serum concentrations of methotrexate and/or its metabolite hydroxymethotrexate; possible methotrexate toxicity1 34 333 334 Reported mainly with high-dose methotrexate (300 mg/m2 to 12 g/m2),1 34 333 but also reported with low dosages (e.g., 15 mg per week)333 |
Manufacturer of esomeprazole recommends considering temporary discontinuance of proton-pump inhibitor therapy in some patients receiving high-dose methotrexate1 34 Some clinicians recommend withholding the proton-pump inhibitor for several days before and after administration of either high-dose or low-dose methotrexate or, alternatively, substituting a histamine H2-receptor antagonist for the proton-pump inhibitor333 334 |
|
Nelfinavir |
Omeprazole decreased peak plasma concentrations and AUCs of nelfinavir and its major active metabolite1 34 347 |
Concomitant use of nelfinavir with proton-pump inhibitors not recommended1 34 |
|
NSAIAs (naproxen, rofecoxib) |
||
|
Oral contraceptives |
||
|
Phenytoin |
||
|
Quinidine |
||
|
Raltegravir |
Omeprazole increased peak plasma concentration and AUC of raltegravir32 348 |
No dosage adjustment recommended when proton-pump inhibitors used with raltegravir32 348 |
|
Rifampin |
||
|
Rilpivirine |
Omeprazole decreased plasma concentrations and AUC of rilpivirine32 343 |
Concomitant use of rilpivirine and proton-pump inhibitors contraindicated32 343 |
|
Saquinavir |
Ritonavir-boosted saquinavir: Omeprazole increased peak plasma concentration and AUC of saquinavir1 32 34 346 |
Caution advised if proton-pump inhibitor used with ritonavir-boosted saquinavir; monitor for saquinavir toxicity1 32 34 346 Manufacturer of esomeprazole recommends considering saquinavir dosage reduction on an individual basis1 34 |
|
St. John’s wort (Hypericum perforatum) |
||
|
Sucralfate |
Possible delayed proton-pump inhibitor absorption and decreased bioavailability 47 |
Administer proton-pump inhibitor at least 30 minutes before sucralfate47 |
|
Tacrolimus |
||
|
Tests for neuroendocrine tumors |
Increased serum chromogranin A (CgA) concentrations (secondary to esomeprazole-induced increase in intragastric pH) may produce false-positive results1 34 |
Temporarily discontinue esomeprazole before assessing CgA concentrations and consider repeating test if initial CgA concentrations are high1 34 |
|
Voriconazole |
Esomeprazole dosage adjustment usually not required but may be considered in patients receiving high dosages (up to 240 mg daily), such as those with Zollinger-Ellison syndrome1 34 |
|
|
Warfarin |
Potential for decreased warfarin metabolism and changes in prothrombin measures1 34 |
Esomeprazole Pharmacokinetics
Absorption
Bioavailability
Delayed-release esomeprazole: Bioavailability is 64% after a single 40-mg oral dose.1 Bioavailability is 90% after repeated oral doses of 40 mg once daily.1
Food
Delayed-release esomeprazole: AUC decreased by 43–53% when a 40-mg oral dose was administered with food.1
Immediate-release esomeprazole/delayed-release naproxen tablets: Administration with high-fat food decreases rate and extent of esomeprazole absorption (peak plasma concentration delayed by 1 hour, AUC decreased 52%, peak concentration decreased 74%).342 Administration 30 minutes before high-fat food does not substantially alter rate or extent of esomeprazole absorption relative to fasted state.342 Administration 1 hour before high-fat food increases esomeprazole AUC and peak concentration by 25 and 50%, respectively, but peak concentration is lower than that observed with labeled dosage of esomeprazole 40 mg daily.342
Special Populations
Following oral dosage of 40 mg once daily in patients with severe (Child-Pugh class C) hepatic impairment, steady-state AUCs were 2–3 times greater than those in patients with normal hepatic function.1 34
Distribution
Extent
Not known whether esomeprazole is distributed into milk, but omeprazole is distributed into milk.1 34 Not known whether esomeprazole crosses the placenta.1 34
Prolonged binding to gastric parietal proton pump enzyme.1 6
Plasma Protein Binding
Elimination
Metabolism
Metabolized to inactive metabolites in the liver by CYP isoenzymes, principally by CYP2C19, and to lesser extent by CYP3A4.1 34
Elimination Route
Excreted principally in urine (80% as inactive metabolites, <1% as active drug); remainder in feces as inactive metabolites.1 34
Half-life
Adults, oral administration: 1–1.5 hours.1 Slower elimination than R-omeprazole or racemic omeprazole (0.5–1 hour).1 5 6
Adults, IV administration: 1.1–1.4 hours; prolonged with increasing dose.34
Adolescents 12–17 years of age, oral administration: 0.8–1.2 hours.1
Children 1–11 years of age, oral administration: 0.7–0.9 hours.1
Infants 1–11 months of age, oral administration: 0.9 hours.1
Special Populations
In patients with poor CYP2C19 metabolizer phenotype, steady-state AUCs were 2 times greater than those in patients with extensive (or rapid) metabolizer phenotype.1 34
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C) in tightly-closed containers.1
Fixed-combination Tablet (Vimovo)
25°C (may be exposed to 15–30°C) in tightly-closed containers.342
Powder for Oral Suspension
25°C (may be exposed to 15–30°C).1
Parenteral
Powder for IV Injection or Infusion
Powder: 25°C (may be exposed to 15–30°C).34 Protect from light.34
Reconstituted solution: Room temperature (up to 30°C) for up to 12 hours.34
Admixture: Room temperature (up to 30°C) for up to 6 hours (in 50 mL of 5% dextrose injection) or 12 hours (in 50 mL of lactated Ringer’s or 0.9% sodium chloride injection).34
Compatibility
Oral
Capsules
Use extemporaneous mixture of capsule contents (enteric-coated pellets) and applesauce immediately; do not store for future use.1 Applesauce should not be hot.1
Parenteral
Solution Compatibility34 HID
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Doripenem |
Actions
-
Inhibits basal and stimulated gastric acid secretion.1 2 7 8 9
-
Concentrates in acid conditions of parietal cell secretory canaliculi; forms active sulfonamide metabolite that irreversibly binds to and inactivates hydrogen-potassium ATPase (proton- or acid pump), blocking final step in secretion of hydrochloric acid.1 2 4 7 8 9 10 34 Acid secretion is inhibited until additional hydrogen-potassium ATPase is synthesized, resulting in prolonged duration of action.2 4 7 8 9 10
-
More esomeprazole reaches and blocks proton pump than does R-omeprazole; therefore, provides greater intragastric pH control than racemic omeprazole.1 5
-
Suppresses H. pylori in patients with duodenal ulcer and/or reflux esophagitis who are infected with the organism.2 Combined therapy with esomeprazole and appropriate anti-infectives (i.e., amoxicillin, clarithromycin) can effectively eradicate H. pylori gastric infection.1 2
Advice to Patients
-
Importance of swallowing capsule intact, without crushing or chewing.1
-
Importance of taking 1 hour before a meal.1
-
If capsule contents are mixed with applesauce for administration, importance of applesauce being soft enough to swallow without chewing.1 Importance of not using hot applesauce.1 Importance of immediately swallowing mixture without crushing or chewing;1 do not store for later use.1
-
If oral suspension is used, importance of mixing packet contents with an appropriate amount of water, allowing mixture to thicken for 2–3 minutes, and then drinking mixture (without crushing or chewing the granules) within 30 minutes of preparation.1
-
Importance of advising patients that use of multiple daily doses of the drug for an extended period of time may increase the risk of fractures of the hip, wrist, or spine.1 305
-
Risk of hypomagnesemia; importance of immediately reporting and seeking care for any cardiovascular or neurologic manifestations (e.g., palpitations, dizziness, seizures, tetany).1
-
Possible increased risk of Clostridium difficile infection; importance of contacting a clinician if persistent watery stools, abdominal pain, and fever occur.335
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.1 Antacids may be used concomitantly as needed for pain relief.1
-
Importance of women informing their clinicians if they are or plan to become pregnant or plan to breast-feed.1 34
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
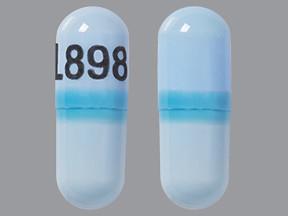
Capsules, delayed-release (containing enteric-coated pellets) |
20 mg (of esomeprazole) |
NexIUM |
AstraZeneca |
|
40 mg (of esomeprazole) |
NexIUM |
AstraZeneca |
||
|
For suspension, delayed-release (containing enteric-coated granules) |
2.5 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
|
|
5 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
||
|
10 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
||
|
20 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
||
|
40 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release core (naproxen only) |
20 mg (of esomeprazole) with Naproxen 375 mg |
Vimovo |
AstraZeneca |
|
20 mg (of esomeprazole) with Naproxen 500 mg |
Vimovo |
AstraZeneca |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for IV use |
20 mg (of esomeprazole) |
NexIUM I.V. |
AstraZeneca |
|
40 mg (of esomeprazole) |
NexIUM I.V. |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 31, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. AstraZeneca. Nexium (esomeprazole magnesium) delayed-release capsules prescribing information. Wilmington, DE; 2012 Jan.
2. McTavish D, Buckley MM, Heel RC. Omeprazole. An updated review of its pharmacology and therapeutic use in acid-related disorders. Drugs. 1991; 42:138-70. http://www.ncbi.nlm.nih.gov/pubmed/1718683?dopt=AbstractPlus
3. Richardson P, Hawkey CJ, Stack WA. Proton pump inhibitors. Pharmacology and rationale for use in gastrointestinal disorders. Drugs. 1998; 56:307-35. http://www.ncbi.nlm.nih.gov/pubmed/9777309?dopt=AbstractPlus
4. Lindberg P, Brändström A, Björn W et al. Omeprazole: The first proton pump inhibitor. Med Res Rev. 1990; 10:1-54.
5. Thitiphuree S, Talley NJ. Esomeprazole, a new proton pump inhibitor: Pharmacological characteristics and clinical efficacy. Int J Clin Pract. 2000; 54:537-41. http://www.ncbi.nlm.nih.gov/pubmed/11198734?dopt=AbstractPlus
6. Astra Merck. Prilosec (omeprazole) delayed-release capsules prescribing information. Wayne, PA; 1998 Jun.
7. Massoomi F, Savage J, Destache CJ. Omeprazole: a comprehensive review. Pharmacotherapy. 1993; 13:46- 59. http://www.ncbi.nlm.nih.gov/pubmed/8437967?dopt=AbstractPlus
8. Howden CW. Clinical pharmacology of omeprazole. Clin Pharmacokinet. 1991; 20:38-49. http://www.ncbi.nlm.nih.gov/pubmed/2029801?dopt=AbstractPlus
9. Shamburek RD, Schubert ML. Pharmacology of gastric acid inhibition. Balilliere’s Clin Gastroenterol. 1993; 7:23-54.
10. Maton PN. Omeprazole. N Engl J Med. 1991; 324:965-75. http://www.ncbi.nlm.nih.gov/pubmed/2002819?dopt=AbstractPlus
11. Sontag SJ, Hirschowitz BI, Holt S et al. Two doses of omeprazole versus placebo in symptomatic erosive esophagitis: the U.S. multicenter study. Gastroenterology. 1992; 102:109-118. http://www.ncbi.nlm.nih.gov/pubmed/1727744?dopt=AbstractPlus
12. Eisai Inc. and Janssen Pharmaceutica Inc. AcipHex (rabeprazole sodium) delayed-release tablets prescribing information. Teaneck and Titusville, NJ; 1999 Aug.
13. Prakash A, Faulds D. Rabeprazole. Drugs. 1998; 55:261-7. http://www.ncbi.nlm.nih.gov/pubmed/9506245?dopt=AbstractPlus
14. Dekkers CP, Beker JA, Thjodleifsson B et al for the European Rabeprazole Study Group. Double-blind comparison (correction of double-blind, placebo-controlled comparison) of rabeprazole 20 mg vs. omeprazole 20 mg in the treatment of erosive or ulcerative gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 1999; 13:49-57. http://www.ncbi.nlm.nih.gov/pubmed/9892879?dopt=AbstractPlus
15. National Institutes of Health Consensus Development Group. Gastroesophageal reflux disease (hiatal hernia and heartburn). NIH Publication No. 94-882; 1994 Sep.
16. Cloud ML, Enas N, Humphries TJ et al for the Rabeprazole Study Group. Rabeprazole in treatment of acid peptic diseases: results of three placebo-controlled dose-response clinical trials in duodenal ulcer, gastric ulcer, and gastroesophageal reflux disease (GERD). Dig Dis Sci. 1998; 43:993-1000. http://www.ncbi.nlm.nih.gov/pubmed/9590413?dopt=AbstractPlus
17. Graul A, Castaner R, Castaner J. Esomeprazole magnesium. Drugs Future. 1999; 24:1178-83.
18. Kahrilas PJ, Falk GW, Johnson DA et al for the Esomeprazole Study Investigators. Esomeprazole improves healing and symptom resolution as compared with omeprazole in reflux oesophagitis patients: A randomized controlled trial. Aliment Pharmacol Ther. 2000; 14:1249-58. http://www.ncbi.nlm.nih.gov/pubmed/11012468?dopt=AbstractPlus
19. Spencer CM, Faulds D. Esomeprazole. Drugs. 2000; 60:321-9. http://www.ncbi.nlm.nih.gov/pubmed/10983736?dopt=AbstractPlus
20. AstraZeneca, Frazer, PA: Personal communication.
21. DeVault KR, Castell DO, Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol. 1999; 94:1434-42. http://www.ncbi.nlm.nih.gov/pubmed/10364004?dopt=AbstractPlus
22. Hanauer SB, Sandborn W, and the Practice Parameters Committee of the American College of Gastroenterology. Management of Crohn’s disease in adults: Practice Guidelines. Am J Gastroenterol. 2001; 96:635-43. http://www.ncbi.nlm.nih.gov/pubmed/11280528?dopt=AbstractPlus
23. Valori RM, Cockel R. Omeprazole for duodenal ulceration in Crohn’s disease. Br Med J. 1990; 300:438-9.
24. Bianchi G, Ardizzone S, Petrillo M et al. Omeprazole for peptic ulcer in Crohn’s disease. Am J Gastroenterol. 1991; 86: 245-6. http://www.ncbi.nlm.nih.gov/pubmed/1992643?dopt=AbstractPlus
25. Przemioslo RT, Mee AS. Omeprazole in possible esophageal Crohn’s disease. Dig Dis Sci. 1994; 39:1594-5. http://www.ncbi.nlm.nih.gov/pubmed/8026276?dopt=AbstractPlus
26. Dickinson JB. Is omeprazole helpful in inflammatory bowel disease? J Clin Gastroenterol. 1994; 18:317-9.
27. Abrahao LJ Jr., Abrahao LJ, Vargas C et al. [Gastoduodenal Crohn’s disease—report of 4 cases and review of the literature]. (Portuguese; with English abstract.) Arq Gastroenterol. 2001; 38:57-62.
28. Freston JW. Review article: role of proton pump inhibitors in non-H. pylori-related ulcers. Aliment Pharmacol Ther. 20001; 15(Suppl 2):2-5.
29. Laheij RJF, Sturkenboom MCJM, Hassing RJ et al. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA. 2004;292:1955-60.
30. Gregor JC. Acid suppression and pneumonia.; a clinical indication for rational prescibing. JAMA. 2004;292:2012-3. Editorial.
31. Bristol-Myers Squibb. Reyataz (atazanavir sulfate) capsules prescribing information. Princeton, NJ; 2012 Mar.
32. Department of Health and Human Services (DHHS) Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (Mar 29, 2012). From the US Department of Health and Human Services HIV/AIDS Information Services (AIDSinfo) website. http://www.aidsinfo.nih.gov/contentfiles/lvguidelines/glchunk/glchunk_32.pdf
33. Scheiman JM, Yeomans ND, Talley NJ et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective NSAIDs and COX-2 inhibitors. Am J Gastroenterol. 2006; 101:701-10. http://www.ncbi.nlm.nih.gov/pubmed/16494585?dopt=AbstractPlus
34. AstraZeneca. Nexium I.V. (esomeprazole sodium) for injection prescribing information. Wilmington, DE; 2012 Jan.
35. Yang Y-X, Lewis JD, Epstein S et al. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006; 296:2947-53. http://www.ncbi.nlm.nih.gov/pubmed/17190895?dopt=AbstractPlus
36. Food and Drug Administration. FDA statement: FDA’s safety reviews of Prilosec and Nexium find no evidence of increased rates of cardiac events. 2007 Dec 10. From the FDA website. Accessed 2007 Dec 21. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm109037.htm
37. Food and Drug Administration. Update of safety review: follow-up to the August 9, 2007, communication about the ongoing safety review of omeprazole and esomeprazole. 2007 Dec 10. From the FDA website. Accessed 2007 Dec 21. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm143258.htm
38. Food and Drug Administration. Early communication about an ongoing safety review: omeprazole (Prilosec) and esomeprazole (Nexium). 2007 Aug 9. From the FDA website. Accessed 2007 Dec 21. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm072497.htm
39. Metz DC, Sostek MB, Ruszniewski P et al. Effects of esomeprazole on acid output in patients with Zollinger-Ellison syndrome or idiopathic gastric acid hypersecretion. Am J Gastroenterol. 2007; 102:2648-54. http://www.ncbi.nlm.nih.gov/pubmed/17764495?dopt=AbstractPlus
40. Gilard M, Arnaud B, Cornily JC et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin. JACC. 2008; 51:256-60, doi:10.1016/j.jacc.2007.06.064. Accessed 2008 Dec 8. Available from website. http://content.onlinejacc.org/cgi/content/abstract/51/3/256 http://www.ncbi.nlm.nih.gov/pubmed/18206732?dopt=AbstractPlus
41. Pezalla E, Day D, Pulliadath I. Initial assessment of clinical impact of a drug interaction between clopidogrel and proton pump inhibitors. JACC. 2008; 52:1038-9. Letter. http://www.ncbi.nlm.nih.gov/pubmed/18786491?dopt=AbstractPlus
42. MEDCO. New study: A common class of GI medications reduce protection against heart attack in patients taking widely prescribed cardiovascular drug. Franklin Lakes, NJ; 2008 Nov 11. Press release from website. http://www.medco.com
43. Gilard M, Cornily JC, Boschat J. Initial assessment of clinical impact of a drug interaction between clopidogrel and proton pump inhibitors. JACC. 2008; 52:1039. Reply.
44. . PPI interactions with clopidogrel revisited. Med Lett Drugs Ther. 2009; 51:13-4.
45. Juurlink DN, Gomes T, Ko DT et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009; 180:713-8. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2659819&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/19176635?dopt=AbstractPlus
46. Food and Drug Administration. Information on clopidogrel bisulfate (marketed as Plavix). Rockville, MD; 2010 Oct 27. From FDA website. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm190836.htm
47. TAP. Prevacid (lansoprazole) delayed-release capsules, for delayed-release oral suspension and delayed-release orally disintegrating tablets prescribing information. Lake Forest, IL; 2011 Jun.
48. US Food and Drug Administration. Center for Drug Evaluation and Research. Application number 021689/S-017: Clinical review. From FDA website. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/UCM258683.pdf
224. Sanofi-Aventis/Bristol-Myers Squibb. Plavix, (clopidogrel bisulfate) tablets prescribing information. New York, NY; 2011 Dec.
225. Food and Drug Administration. Early communication about an ongoing safety review of clopidogrel bisulfate (marketed as Plavix). Rockville, MD; 2009 Jan 26. From FDA website. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm079520.htm
226. Siller-Matula JM, Spiel AO, Lang IM et al. Effects of pantoprazole and esomeprazole on platelet inhibition by clopidogrel. Am Heart J. 2009; 157:148.e1-5.
227. Gilard M, Arnaud B, Le Gal G et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated to aspirin. J Thromb Haemost. 2006; 4:2508-9. http://www.ncbi.nlm.nih.gov/pubmed/16898956?dopt=AbstractPlus
228. Anon. PPI interactions with clopidogrel. Med Lett Drugs Ther. 2009; 51:2-3.
229. Aubert RE, Epstein RS, Teagarden JR et al. Proton pump inhibitors effect on clopidogrel effectiveness: The clopidogrel Medco outcomes study. Circulation. 2008; 118:S_815, Abstract 3998.
230. Lau WC, Gurbel PA. The drug-drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009; 180:699-700. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2659824&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/19332744?dopt=AbstractPlus
232. Food and Drug Administration. Information for heathcare professionals: Update to the labeling of clopidogrel bisulfate (marketed as Plavix) to alert heathcare professionals about a drug interaction with omeprazole (marketed as Prilosec and Prilosec OTC). Rockville, MD; 2009 Nov 17. From FDA website. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm190787.htm
233. Food and Drug Administration. Follow-up to the January 26, 2009 Early Communication about an ongoing safety review of clopidogrel bisulfate (marketed as Plavix) and omeprazole (marketed as Prilosec and Prilosec OTC). Rockville, MD; 2009 Nov 17. From FDA website. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm190784.htm
235. Ho PM, Maddox TM, Wang L et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009; 301:937-44. http://www.ncbi.nlm.nih.gov/pubmed/19258584?dopt=AbstractPlus
236. Norgard NB, Mathews KD, Wall GC. Drug-drug interaction between clopidogrel and the proton pump inhibitors. Ann Pharmacother. 2009; 43:1266-74. http://www.ncbi.nlm.nih.gov/pubmed/19470853?dopt=AbstractPlus
237. Last EJ, Sheehan AH. Review of recent evidence: potential interaction between clopidogrel and proton pump inhibitors. Am J Health Syst Pharm. 2009; 66:2117-22. http://www.ncbi.nlm.nih.gov/pubmed/19923312?dopt=AbstractPlus
238. Stanek EJ, Aubert RE, Flockhart DA et al. A national study of the effect of individual proton pump inhibitors on cardiovascular outcomes in patients treated with clopidogrel following coronary stenting: the Clopidogrel Medco Outcomes Study. Available from website. Accessed 2009 Dec 15. http://www.theheart.org/displayItem.do?primaryKey=967345&type=ppt
240. Stockl KM, Le L, Zakharyan A et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med. 2010; 170:704-10. http://www.ncbi.nlm.nih.gov/pubmed/20421557?dopt=AbstractPlus
243. Juurlink DN. Proton pump inhibitors and clopidogrel: putting the interaction in perspective. Circulation. 2009; 120:2310-2. http://www.ncbi.nlm.nih.gov/pubmed/19933929?dopt=AbstractPlus
248. Khalique SC, Cheng-Lai A. Drug interaction between clopidogrel and proton pump inhibitors. Cardiol Rev. 2009 Jul-Aug; 17:198-200.
250. Rude MK, Chey WD. Proton-pump inhibitors, clopidogrel, and cardiovascular adverse events: fact, fiction, or something in between?. Gastroenterology. 2009; 137:1168-71. http://www.ncbi.nlm.nih.gov/pubmed/19635603?dopt=AbstractPlus
300. Vestergaard P, Rejnmark L, Mosekilde L. Proton pump inhibitors, histamine H2 receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int. 2006; 79:76-83. http://www.ncbi.nlm.nih.gov/pubmed/16927047?dopt=AbstractPlus
301. Corley DA, Kubo A, Zhao W et al. Proton pump inhibitors and histamine-2 receptor antagonists are associated with hip fractures among at-risk patients. Gastroenterology. 2010; 139:93-101. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2902649&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/20353792?dopt=AbstractPlus
302. Yu EW, Blackwell T, Ensrud KE et al. Acid-suppressive medications and risk of bone loss and fracture in older adults. Calcif Tissue Int. 2008; 83:251-9. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2596870&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/18813868?dopt=AbstractPlus
303. Gray SL, LaCroix AZ, Larson J et al. Proton pump inhibitor use, hip fracture, and change in bone mineral density in postmenopausal women: results from the Women’s Health Initiative. Arch Intern Med. 2010; 170:765-71. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=4240017&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/20458083?dopt=AbstractPlus
304. Targownik LE, Lix LM, Metge CJ et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008; 179:319-26. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2492962&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/18695179?dopt=AbstractPlus
305. Food and Drug Administration. Possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors. May 25, 2010. From FDA web site. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm213206.htm
307. Yang YX, Metz DC. Safety of proton pump inhibitor exposure. Gastroenterology. 2010; :.
308. Targownik LE, Lix LM, Leung S et al. Proton-pump inhibitor use is not associated with osteoporosis or accelerated bone mineral density loss. Gastroenterology. 2010; 138:896-904. http://www.ncbi.nlm.nih.gov/pubmed/19931262?dopt=AbstractPlus
310. Kaye JA, Jick H. Proton pump inhibitor use and risk of hip fractures in patients without major risk factors. Pharmacotherapy. 2008; 28:951-9. http://www.ncbi.nlm.nih.gov/pubmed/18657011?dopt=AbstractPlus
311. Abraham NS, Hlatky MA, Antman EM et al. ACCF/ACG/AHA 2010 Expert Consensus Document on the Concomitant Use of Proton Pump Inhibitors and Thienopyridines: A Focused Update of the ACCF/ACG/AHA 2008 Expert Consensus Document on Reducing the Gastrointestinal Risks of Antiplatelet Therapy and NSAID Use. A report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. JACC. 2010; 56: Published online Nov 8, 2010.
312. Last EJ, Sheehan AH. Review of recent evidence: potential interaction between clopidogrel and proton pump inhibitors. Am J Health Syst Pharm. 2009; 66:2117-22. http://www.ncbi.nlm.nih.gov/pubmed/19923312?dopt=AbstractPlus
313. Stockl KM, Le L, Zakharyan A et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med. 2010; 170:704-10. http://www.ncbi.nlm.nih.gov/pubmed/20421557?dopt=AbstractPlus
314. Juurlink DN. Proton pump inhibitors and clopidogrel: putting the interaction in perspective. Circulation. 2009; 120:2310-2. http://www.ncbi.nlm.nih.gov/pubmed/19933929?dopt=AbstractPlus
315. Khalique SC, Cheng-Lai A. Drug interaction between clopidogrel and proton pump inhibitors. Cardiol Rev. 2009 Jul-Aug; 17:198-200.
316. Rude MK, Chey WD. Proton-pump inhibitors, clopidogrel, and cardiovascular adverse events: fact, fiction, or something in between?. Gastroenterology. 2009; 137:1168-71. http://www.ncbi.nlm.nih.gov/pubmed/19635603?dopt=AbstractPlus
317. Furlanetto TW, Faulhaber GA. Hypomagnesemia and Proton Pump Inhibitors: Below the Tip of the Iceberg. Arch Intern Med. 2011; :. http://www.ncbi.nlm.nih.gov/pubmed/21555654?dopt=AbstractPlus
318. Fernández-Fernández FJ, Sesma P, Caínzos-Romero T et al. Intermittent use of pantoprazole and famotidine in severe hypomagnesaemia due to omeprazole. Neth J Med. 2010; 68:329-30. http://www.ncbi.nlm.nih.gov/pubmed/21071783?dopt=AbstractPlus
319. Mackay JD, Bladon PT. Hypomagnesaemia due to proton-pump inhibitor therapy: a clinical case series. QJM. 2010; 103:387-95. http://www.ncbi.nlm.nih.gov/pubmed/20378675?dopt=AbstractPlus
320. Shabajee N, Lamb EJ, Sturgess I et al. Omeprazole and refractory hypomagnesaemia. BMJ. 2008; 337:a425. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2483862&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/18617497?dopt=AbstractPlus
321. . In brief: PPI’s and hypomagnesemia. Med Lett Drugs Ther. 2011; 53:25.
322. Cundy T, Dissanayake A. Severe hypomagnesaemia in long-term users of proton-pump inhibitors. Clin Endocrinol (Oxf). 2008; 69:338-41. http://www.ncbi.nlm.nih.gov/pubmed/18221401?dopt=AbstractPlus
323. Broeren MA, Geerdink EA, Vader HL et al. Hypomagnesemia induced by several proton-pump inhibitors. Ann Intern Med. 2009; 151:755-6. http://www.ncbi.nlm.nih.gov/pubmed/19920278?dopt=AbstractPlus
324. Metz DC, Sostek MB, Ruszniewski P et al. Effects of esomeprazole on acid output in patients with Zollinger-Ellison syndrome or idiopathic gastric acid hypersecretion. Am J Gastroenterol. 2007; 102:2648-54. http://www.ncbi.nlm.nih.gov/pubmed/17764495?dopt=AbstractPlus
325. Kuipers MT, Thang HD, Arntzenius AB. Hypomagnesaemia due to use of proton pump inhibitors--a review. Neth J Med. 2009; 67:169-72. http://www.ncbi.nlm.nih.gov/pubmed/19581665?dopt=AbstractPlus
326. Epstein M, McGrath S, Law F. Proton-pump inhibitors and hypomagnesemic hypoparathyroidism. N Engl J Med. 2006; 355:1834-6. http://www.ncbi.nlm.nih.gov/pubmed/17065651?dopt=AbstractPlus
327. US Food and Drug Administration. FDA drug safety communication: Low magnesium levels can be associated with long-term use of proton pump inhibitor drugs (PPIs). Rockville, MD; 2011 March 2. From FDA website. http://www.fda.gov/Drugs/DrugSafety/ucm245011.htm
328. US Food and Drug Administration. Proton pump inhibitor drugs (PPIs): Drug safety communication- Low magnesium levels can be associated with long-term use. Rockville, MD; 2011 March 2. From FDA website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm245275.htm
329. Hoorn EJ, van der Hoek J, de Man RA et al. A case series of proton pump inhibitor-induced hypomagnesemia. Am J Kidney Dis. 2010; 56:112-6. http://www.ncbi.nlm.nih.gov/pubmed/20189276?dopt=AbstractPlus
330. Regolisti G, Cabassi A, Parenti E et al. Severe hypomagnesemia during long-term treatment with a proton pump inhibitor. Am J Kidney Dis. 2010; 56:168-74. http://www.ncbi.nlm.nih.gov/pubmed/20493607?dopt=AbstractPlus
331. GlaxoSmithKline. Lanoxin (digoxin) tablets prescribing information. Research Triangle Park, NC; 2009 Aug.
333. Bezabeh S, Mackey AC, Kluetz P et al. Accumulating evidence for a drug-drug interaction between methotrexate and proton pump inhibitors. Oncologist. 2012; 17:550-4. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3336837&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/22477728?dopt=AbstractPlus
334. Horn JR, Hansten PD. Methotrexate and proton pump inhibitors. Pharm Times. 2012; 78(4). Published online 2012 Apr 9. http://www.pharmacytimes.com/publications/issue/2012/April2012/Methotrexate-and-Proton-Pump-Inhibitors
335. Food and Drug Administration. Drug safety communication: Clostridium difficile-associated diarrhea can be associated with stomach acid drugs known as proton pump inhibitors (PPIs). Rockville, MD; 2012 Feb 8. From FDA website. Accessed 2012 May 3l. http://www.fda.gov/Drugs/DrugSafety/ucm290510.htm
336. Cohen SH, Gerding DN, Johnson S et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431-55. http://www.ncbi.nlm.nih.gov/pubmed/20307191?dopt=AbstractPlus
337. Shah S, Lewis A, Leopold D et al. Gastric acid suppression does not promote clostridial diarrhoea in the elderly. QJM. 2000; 93:175-81. http://www.ncbi.nlm.nih.gov/pubmed/10751237?dopt=AbstractPlus
338. Leonard AD, Ho KM, Flexman J. Proton pump inhibitors and diarrhoea related to Clostridium difficile infection in hospitalised patients: a case-control study. Intern Med J. 2012; 42:591-4. http://www.ncbi.nlm.nih.gov/pubmed/22616966?dopt=AbstractPlus
339. Kwok CS, Arthur AK, Anibueze CI et al. Risk of Clostridium difficile Infection With Acid Suppressing Drugs and Antibiotics: Meta-Analysis. Am J Gastroenterol. 2012; 107:1011-9. http://www.ncbi.nlm.nih.gov/pubmed/22525304?dopt=AbstractPlus
340. Dial S, Delaney JA, Barkun AN et al. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005; 294:2989-95. http://www.ncbi.nlm.nih.gov/pubmed/16414946?dopt=AbstractPlus
341. Nerandzic MM, Pultz MJ, Donskey CJ. Examination of potential mechanisms to explain the association between proton pump inhibitors and Clostridium difficile infection. Antimicrob Agents Chemother. 2009; 53:4133-7. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2764230&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/19667292?dopt=AbstractPlus
342. AstraZeneca. Vimovo (naproxen/esomeprazole magnesium) delayed-release tablets prescribing information. Wilmington, DE; 2010 Apr.
343. Tibotec Therapeutics. Edurant (rilpivirine) tablets prescribing information. Raritan, NJ; 2011 May.
344. Abbott Laboratories. Kaletra (lopinavir/ritonavir) oral tablets and solution prescribing information. North Chicago, IL; 2012 May.
345. ViiV Healthcare. Lexiva (fosamprenavir calcium) tablets and oral suspension prescribing information. Research Triangle Park, NC; 2012 Apr.
346. Genentech USA. Invirase (saquinavir mesylate) capsules and tablets prescribing information. South San Francisco, CA; 2012 Feb.
347. ViiV Healthcare. Viracept (nelfinavir mesylate) tablets and oral powder prescribing information. Research Triangle Park, NC; 2012 Apr.
348. Merck Sharp & Dohme. Isentress (raltegravir) film-coated tablets and chewable tablets prescribing information. Whitehouse Station, NJ; 2012 Apr.
350. Frelinger AL, Lee RD, Mulford DJ et al. A randomized, 2-period, crossover design study to assess the effects of dexlansoprazole, lansoprazole, esomeprazole, and omeprazole on the steady-state pharmacokinetics and pharmacodynamics of clopidogrel in healthy volunteers. J Am Coll Cardiol. 2012; 59:1304-11. http://www.ncbi.nlm.nih.gov/pubmed/22464259?dopt=AbstractPlus
351. Angiolillo DJ, Gibson CM, Cheng S et al. Differential effects of omeprazole and pantoprazole on the pharmacodynamics and pharmacokinetics of clopidogrel in healthy subjects: randomized, placebo-controlled, crossover comparison studies. Clin Pharmacol Ther. 2011; 89:65-74. http://www.ncbi.nlm.nih.gov/pubmed/20844485?dopt=AbstractPlus
HID. Trissel LA. Handbook on injectable drugs. 16th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2011:615-16.
Frequently asked questions
More about esomeprazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (267)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: proton pump inhibitors
- Breastfeeding
Patient resources
Professional resources
- Esomeprazole prescribing information
- Esomeprazole Capsules (FDA)
- Esomeprazole Injection (FDA)
- Esomeprazole Oral Suspension (FDA)
- Esomeprazole Strontium Capsules (FDA)