Cycloserine (Monograph)
Brand name: Seromycin
Drug class: Antituberculosis Agents
- Antimycobacterial Agents
VA class: AM500
CAS number: 68-41-7
Introduction
Antituberculosis agent; structural analog of the amino acid d-alanine.
Uses for Cycloserine
Tuberculosis
Treatment of active (clinical) tuberculosis (TB) in conjunction with other antituberculosis agents.
Second-line agent used in treatment of drug-resistant TB caused by Mycobacterium tuberculosis known or presumed to be susceptible to cycloserine.
For initial treatment of active TB caused by drug-susceptible M. tuberculosis, recommended multiple-drug regimens consist of an initial intensive phase (2 months) and a continuation phase (4 or 7 months). Although the usual duration of treatment for drug-susceptible pulmonary and extrapulmonary TB (except disseminated infections and TB meningitis) is 6–9 months, ATS, CDC, and IDSA state that completion of treatment is determined more accurately by the total number of doses and should not be based solely on the duration of therapy. A longer duration of treatment (e.g., 12–24 months) usually is necessary for infections caused by drug-resistant M. tuberculosis.
Patients with treatment failure or drug-resistant M. tuberculosis, including multidrug-resistant (MDR) TB (resistant to both isoniazid and rifampin) or extensively drug-resistant (XDR) TB (resistant to both isoniazid and rifampin and also resistant to a fluoroquinolone and at least one parenteral second-line antimycobacterial such as capreomycin, kanamycin, or amikacin), should be referred to or managed in consultation with experts in the treatment of TB as identified by local or state health departments or CDC.
Urinary Tract Infections (UTIs)
Has been used for treatment of acute UTIs caused by susceptible gram-positive or -negative bacteria, especially Enterobacter or Escherichia coli. No longer recommended; generally less effective than other antibacterials available for treatment of UTIs.
Should be used for treatment of UTIs only when other more effective and less toxic alternatives are contraindicated and susceptibility to cycloserine has been demonstrated.
Cycloserine Dosage and Administration
Administration
Oral Administration
Administer orally.
Dosage
Should not be used alone for treatment of active (clinical) TB; must be given in conjunction with other antituberculosis agents.
Data not available to date to support use of cycloserine in intermittent (e.g., 1-3 times weekly) multiple-drug TB regimens.
Pediatric Patients
Tuberculosis
Treatment of Active (Clinical) Tuberculosis
OralChildren <15 years of age or weighing ≤40 kg† [off-label]: 10–20 mg/kg daily (up to 1 g daily) given in 2 divided doses recommended by ATS, CDC, IDSA, and AAP.
Children ≥15 years of age† [off-label]: 10–15 mg/kg daily (up to 1 g daily) given in 2 divided doses recommended by ATS, CDC, and IDSA. Usual dosage is 500–750 mg daily given in 2 divided doses; toxicity is more common with dosages >500 mg daily. These experts suggest optimum dosage usually can be determined by maintaining peak cycloserine serum concentrations at 20–35 mcg/mL.
Adults
Tuberculosis
Treatment of Active (Clinical) Tuberculosis
Oral10–15 mg/kg daily (up to 1 g daily) given in 2 divided doses recommended by ATS, CDC, and IDSA. Usual dosage is 500–750 mg daily given in 2 divided doses; toxicity is more common with dosages >500 mg daily. These experts suggest optimum dosage usually can be determined by maintaining peak cycloserine serum concentrations at 20–35 mcg/mL.
Manufacturer states usual initial dosage is 250 mg every 12 hours for the first 2 weeks. Usual dosage is 0.5–1 g daily given in divided doses with serum concentration monitoring. Manufacturer recommends dosage be adjusted to maintain serum concentrations <30 mcg/mL.
Urinary Tract Infections (UTIs)
Acute UTIs
Oral250 mg every 12 hours for 2 weeks.
Prescribing Limits
Pediatric Patients
Tuberculosis
Treatment of Active (Clinical) Tuberculosis
OralMaximum 1 g daily.
Adults
Tuberculosis
Treatment of Active (Clinical) Tuberculosis
OralMaximum 1 g daily.
Special Populations
Renal Impairment
Contraindicated in severe renal insufficiency. In other patients, adjust dosage according to degree of renal impairment and monitor serum cycloserine concentrations. Maintain serum cycloserine concentrations <30 mcg/mL. (See Renal Impairment under Cautions.)
ATS, CDC, and IDSA state the drug should not be used in patients with Clcr <50 mL/minute unless they are undergoing hemodialysis. For those being treated for TB who are undergoing hemodialysis, these experts suggest a dosage of 500 mg 3 times weekly or 250 mg once daily (with close monitoring of serum cycloserine concentrations).
Cautions for Cycloserine
Contraindications
-
Hypersensitivity to cycloserine.
-
History of epilepsy, depression, severe anxiety, or psychosis.
-
Severe renal insufficiency. (See Renal Impairment under Cautions.)
-
Excessive concurrent use of alcohol. (See CNS Effects under Cautions.)
Warnings/Precautions
Warnings
CNS Effects
CNS effects are the most frequent adverse effects. Drowsiness, somnolence, dizziness, headache, lethargy, depression, tremor, dysarthria, hyperreflexia, paresthesia, nervousness, anxiety, vertigo, confusion and disorientation (with loss of memory), paresis, major and minor clonic seizures, seizures, and coma have been reported. Psychosis (possibly with suicidal tendencies), personality changes, hyperirritability, and aggression have also occurred.
Increased risk of seizures in chronic alcoholics. (See Interactions.)
Adverse CNS effects appear to be dose related and occur within the first 2 weeks of therapy in about 30% of those receiving 500 mg daily. Determine plasma concentrations at least once weekly in patients receiving >500 mg daily, in patients with reduced renal function, and in those with signs or symptoms of toxicity. Adverse nervous system effects are minimized when plasma cycloserine concentrations are <30 mcg/mL.
Some experts recommend that neuropsychiatric status be assessed at least once monthly and more frequently if symptoms develop. Patients with renal impairment should be closely monitored for evidence of neurotoxicity.
If symptoms of CNS toxicity (e.g., seizures, psychosis, somnolence, depression, confusion, hyperreflexia, headache, tremor, vertigo, paresis, dysarthria) occur, reduce dosage or discontinue cycloserine. Symptoms generally disappear when the drug is discontinued.
Sedatives may be effective in controlling anxiety or tremor; anticonvulsants may control seizures. (See Interactions.)
Value of pyridoxine in preventing cycloserine-associated CNS toxicity has not been proven. Neurotoxic effects may be relieved or prevented by concomitant administration of pyridoxine hydrochloride (100–300 mg daily).
Sensitivity Reactions
Rash and allergic reactions reported. Photosensitivity has occurred.
If allergic dermatitis occurs, reduce dosage or discontinue cycloserine.
General Precautions
Precautions Related to Treatment of Tuberculosis
Should not be used alone for treatment of active (clinical) TB; must be given in conjunction with other antituberculosis agents.
Clinical specimens for microscopic examination and mycobacterial cultures and in vitro susceptibility testing should be obtained prior to initiation of antituberculosis therapy and periodically during treatment to monitor therapeutic response. The antituberculosis regimen should be modified as needed. Patients with positive cultures after 4 months of treatment should be considered to have failed treatment (usually as the result of noncompliance or drug-resistant TB). Cycloserine in vitro susceptibility testing may be technically difficult.
If cycloserine is added as a new drug to a regimen in patients experiencing treatment failure who have proven or suspected drug-resistant TB, at least 2 (preferably 3) new drugs known or expected to be active against the resistant strain should be added at the same time.
Compliance with the full course of antituberculosis therapy and all drugs included in the multiple-drug regimen is critical. Missed doses increase the risk of treatment failure and increase the risk that M. tuberculosis will develop resistance to the antituberculosis regimen.
To ensure compliance, ATS, CDC, IDSA, and AAP recommend that directly observed (supervised) therapy (DOT) be used for treatment of active TB whenever possible, especially when intermittent regimens are used, when the patient is immunocompromised or infected with HIV, or when drug-resistant M. tuberculosis is involved.
Hematologic Effects
Vitamin B12 and/or folic acid deficiency, megaloblastic anemia, and sideroblastic anemia have been reported in patients receiving cycloserine in conjunction with other antituberculosis agents.
If anemia occurs, initiate appropriate studies and therapy.
Laboratory Monitoring
Monitor renal, hepatic, and hematologic function.
Monitor cycloserine concentrations; measure concentrations at least once weekly in those with reduced renal function, in those receiving >500 mg daily, and in those showing signs and symptoms that suggest toxicity. Adjust dosage to maintain serum concentrations <30 mcg/mL.
Specific Populations
Pregnancy
Category C.
Because cycloserine crosses the placenta and data are limited regarding safety of the drug in pregnant women, ATS, CDC, and IDSA state the drug should be used for treatment of TB during pregnancy only when there are no suitable alternatives.
Lactation
Distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children.
ATS, CDC, IDSA, and AAP consider cycloserine one of several second-line antituberculosis agents that can be used in children† [off-label].
Hepatic Impairment
Caution in patients with alcohol-related hepatitis. (See Interactions.)
Renal Impairment
Use caution in patients with renal impairment; contraindicated in those with severe renal insufficiency.
Symptoms of acute toxicity may occur if usual dosage is used in patients with renal impairment. Adjust dosage according to the degree of renal impairment and serum cycloserine concentrations. Closely monitor patients with renal impairment for evidence of neurotoxicity.
Determine serum cycloserine concentrations at least once weekly in patients with reduced renal function; adjust dosage to maintain concentrations <30 mcg/mL. (See CNS Effects under Cautions.)
Common Adverse Effects
CNS effects (seizures, drowsiness, somnolence, dizziness, headache, tremor, dysarthria, hyperreflexia, paresthesia, nervousness, anxiety, vertigo, confusion, disorientation with loss of memory, paresis, coma); hypersensitivity reactions.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Possible increased risk of seizures in chronic alcoholics and other frequent users of alcohol, especially those receiving high cycloserine dosage |
Excessive concurrent use of alcohol contraindicated |
|
Ethionamide |
Possible increased risk of adverse effects; seizures reported |
Use concomitantly with caution |
|
Isoniazid |
Adverse CNS effects (e.g., dizziness, drowsiness) may be additive |
Use concomitantly with caution; monitor closely for signs of CNS toxicity; dosage adjustment may be necessary |
|
Phenytoin |
Cycloserine inhibits hepatic metabolism of phenytoin |
Observe closely for evidence of phenytoin intoxication; monitor phenytoin concentrations; reduce phenytoin dosage if necessary |
Cycloserine Pharmacokinetics
Absorption
Bioavailability
Readily absorbed from GI tract. About 65–90% of an oral dose absorbed; peak plasma concentrations attained within 3–8 hours.
Plasma Concentrations
Plasma concentrations of 25–30 mcg/mL generally are maintained with a dosage of 250 mg twice daily, but relationship between plasma concentrations and dosage not always consistent.
Some drug accumulation may occur in patients with normal renal function during the first 3 days of cycloserine therapy.
Distribution
Extent
Widely distributed into body tissues and fluids including the lungs, ascitic fluid, pleural fluid, lymph tissue, and synovial fluid in concentrations approximately equal to plasma concentrations of the drug. Also distributed into bile, sputum, and lymph tissue.
CSF concentrations are 50–80% of concurrent plasma concentrations in patients with uninflamed meninges and 80–100% of concurrent plasma concentrations in patients with inflamed meninges.
Readily crosses the placenta and is distributed into amniotic fluid.
Distributed into milk in concentrations similar to maternal plasma concentrations.
Plasma Protein Binding
Not bound to plasma proteins.
Elimination
Metabolism
About 35% of a dose appears to be metabolized to unidentified metabolites.
Elimination Route
60–70% of an oral dose excreted unchanged in urine by glomerular filtration within 72 hours. The maximum excretion rate occurs during the first 2–6 hours; approximately 50% of the dose is eliminated within 12 hours. Negligible amounts excreted in feces.
Removed by hemodialysis.
Half-life
Approximately 10 hours in patients with normal renal function.
Special Populations
Half-life prolonged in patients with impaired renal function.
Stability
Storage
Oral
Capsules
20–25°C in tight container.
Destroyed at neutral or acidic pH; deteriorates upon absorbing water.
Actions and Spectrum
-
May be bacteriostatic or bactericidal in action, depending on the concentration of the drug attained at the site of infection and the susceptibility of the infecting organism.
-
Inhibits cell wall synthesis in susceptible organisms by competing with d-alanine for incorporation into the bacterial cell wall. In vitro, antibacterial activity may be inhibited by d-alanine.
-
Spectrum of activity includes mycobacteria and some gram-positive and -negative bacteria.
-
Mycobacteria: Active against M. tuberculosis, M. bovis, and some strains of M. kansasii, M. marinum, M. ulcerans, M. avium complex (MAC), M. smegmatis, and M. intracellulare.
-
Gram-positive and gram-negative bacteria: Active against Staphylococcus aureus, Enterobacter, and Escherichia coli.
-
Natural and acquired resistance to cycloserine demonstrated in vitro and in vivo in strains of M. tuberculosis. No evidence of cross-resistance between cycloserine and other antituberculosis agents available in the US.
Advice to Patients
-
Advise patients that poor compliance with antituberculosis regimens can result in treatment failure and development of drug-resistant TB, which can be life-threatening and lead to other serious health risks.
-
Importance of avoiding excessive concurrent use of alcohol.
-
Importance of notifying clinicians if allergic dermatitis or symptoms of CNS toxicity (seizures, psychosis, somnolence, depression, confusion, hyperreflexia, headache, tremor, vertigo, paresis, dysarthria) occur.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
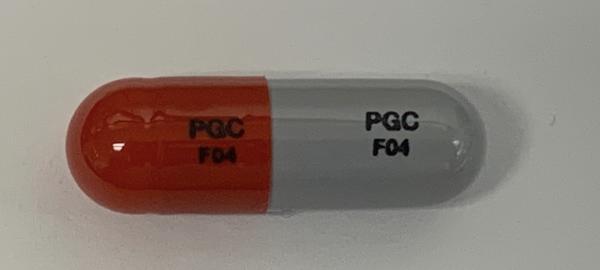
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
250 mg |
Seromycin |
Lilly |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions February 1, 2008. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about cycloserine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: streptomyces derivatives
- Breastfeeding
- En español