Tecvayli Dosage
Generic name: TECLISTAMAB 10mg in 1mL
Dosage form: injection
Drug class: Bispecific T-cell engagers (BiTE)
Medically reviewed by Drugs.com. Last updated on Jul 5, 2024.
Recommended Dosage
For subcutaneous injection only.
The recommended dosing schedule for TECVAYLI is provided in Table 1. The recommended dosage of TECVAYLI is step-up doses of 0.06 mg/kg and 0.3 mg/kg followed by 1.5 mg/kg once weekly until disease progression or unacceptable toxicity. In patients who have achieved and maintained a complete response or better for a minimum of 6 months, the dosing frequency may be decreased to 1.5 mg/kg every two weeks until disease progression or unacceptable toxicity.
Administer pretreatment medications prior to each dose of the TECVAYLI step-up dosing schedule, which includes step-up dose 1, step-up dose 2, and the first treatment dose as described in Table 1 .
Administer TECVAYLI subcutaneously according to the step-up dosing schedule in Table 1 to reduce the incidence and severity of cytokine release syndrome (CRS). Due to the risk of CRS and neurologic toxicity, including ICANS, patients should be hospitalized for 48 hours after administration of all doses within the TECVAYLI step-up dosing schedule .
| Dosing schedule | Day | Dose | |
|---|---|---|---|
|
|||
| All Patients | |||
| Step-up dosing schedule * | Day 1 | Step-up dose 1 | 0.06 mg/kg |
| Day 4 † | Step-up dose 2 | 0.3 mg/kg | |
| Day 7 ‡ | First treatment dose | 1.5 mg/kg | |
| Weekly dosing schedule * | One week after first treatment dose and weekly thereafter | Subsequent treatment doses | 1.5 mg/kg once weekly |
| Patients who have achieved and maintained a complete response or better for a minimum of 6 months | |||
| Biweekly (every two weeks) dosing schedule * | The dosing frequency may be decreased to 1.5 mg/kg every two weeks. | ||
Refer to Tables 7, 8, and 9 to determine the dosage based on predetermined weight ranges .
Recommended Pretreatment Medications
Administer the following pretreatment medications 1 to 3 hours before each dose of the TECVAYLI step-up dosing schedule, which includes step-up dose 1, step-up dose 2, and the first treatment dose (see Table 1), to reduce the risk of CRS .
- Corticosteroid (oral or intravenous dexamethasone 16 mg)
- Histamine-1 (H1) receptor antagonist (oral or intravenous diphenhydramine 50 mg or equivalent)
- Antipyretics (oral or intravenous acetaminophen 650 mg to 1,000 mg or equivalent)
Administration of pretreatment medications may be required prior to administration of subsequent doses of TECVAYLI in the following patients:
- Patients who repeat doses within the TECVAYLI step-up dosing schedule following a dose delay.
- Patients who experienced CRS following the prior dose of TECVAYLI.
Restarting TECVAYLI after Dosage Delay
If a dose of TECVAYLI is delayed, restart therapy based on the recommendations in Table 2 and resume the treatment schedule accordingly . Administer pretreatment medications as indicated in Table 2 .Due to the risk of CRS and neurologic toxicity, including ICANS, patients should be hospitalized for 48 hours after administration of all doses within the TECVAYLI step-up dosing schedule.
| Last dose administered | Time since the last dose administered | Action |
|---|---|---|
| Step-up dose 1 | More than 7 days | Restart TECVAYLI step-up dosing schedule at step-up dose 1 (0.06 mg/kg). * |
| Step-up dose 2 | 8 days to 28 days | Repeat step-up dose 2 (0.3 mg/kg) *and continue TECVAYLI step-up dosing schedule. |
| More than 28 days † | Restart TECVAYLI step-up dosing schedule at step-up dose 1 (0.06 mg/kg). * | |
| Any treatment dose | 28 days or less | Continue TECVAYLI at last treatment dose and schedule (1.5 mg/kg once weekly or 1.5 mg/kg every two weeks; see Table 1). |
| More than 28 days † | Restart TECVAYLI step-up dosing schedule at step-up dose 1 (0.06 mg/kg). * | |
Dosage Modifications for Adverse Reactions
Dosage reductions of TECVAYLI are not recommended.
Dosage delays may be required to manage toxicities related to TECVAYLI.
See Tables 3, 4, and 5for recommended actions for adverse reactions of CRS, neurologic toxicity, and ICANS. See Table 6for recommended actions for other adverse reactions following administration of TECVAYLI.
Management of CRS, Neurologic Toxicity and ICANS
Cytokine Release Syndrome (CRS)
Management recommendations for CRS are summarized in Table 3.
Identify CRS based on clinical presentation. Evaluate and treat other causes of fever, hypoxia, and hypotension.
If CRS is suspected, withhold TECVAYLI until CRS resolves. Manage according to the recommendations in Table 3 and consider further management per current practice guidelines. Administer supportive therapy for CRS, which may include intensive care for severe or life-threatening CRS. Consider laboratory testing to monitor for disseminated intravascular coagulation (DIC), hematology parameters, as well as pulmonary, cardiac, renal, and hepatic function.
| Grade * | Presenting Symptoms | Actions |
|---|---|---|
|
||
| Grade 1 | Temperature ≥100.4°F (38°C) † |
|
| Grade 2 | Temperature ≥100.4°F (38°C) †with: Hypotension responsive to fluids and not requiring vasopressors, and/or, Oxygen requirement of low-flow nasal cannula §or blow-by. |
|
| Grade 3 | Temperature ≥100.4°F (38°C) †with: Hypotension requiring one vasopressor with or without vasopressin, and/or, Oxygen requirement of high-flow nasal cannula §, facemask, non-rebreather mask, or Venturi mask. |
First Occurrence of Grade 3 CRS with Duration Less than 48 Hours: |
Recurrent Grade 3 CRS or Grade 3 CRS with Duration 48 Hours or Longer:
|
||
| Grade 4 | Temperature ≥100.4°F (38°C) †with: Hypotension requiring multiple vasopressors (excluding vasopressin), and/or, Oxygen requirement of positive pressure (e.g., continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), intubation, and mechanical ventilation). |
|
Neurologic Toxicity and ICANS
Management recommendations for neurologic toxicity and ICANS are summarized in Tables 4 and 5.
At the first sign of neurologic toxicity, including ICANS, withhold TECVAYLI and consider neurology evaluation. Rule out other causes of neurologic symptoms. Provide supportive therapy, which may include intensive care, for severe or life-threatening neurologic toxicities, including ICANS . Manage ICANS according to the recommendations in Table 5 and consider further management per current practice guidelines.
| Adverse Reaction | Severity * | Actions |
|---|---|---|
| Neurologic Toxicity *(excluding ICANS) | Grade 1 |
|
| Grade 2 Grade 3 (First occurrence) |
|
|
| Grade 3 (Recurrent) Grade 4 |
|
|
| Grade * | Presenting Symptoms † | Actions |
|---|---|---|
|
||
| Grade 1 | ICE score 7–9 ‡, or depressed level of consciousness §: awakens spontaneously. |
|
| Grade 2 | ICE score 3–6 ‡, or depressed level of consciousness §: awakens to voice. |
|
| Grade 3 | ICE score 0–2 ‡, or depressed level of consciousness §: awakens only to tactile stimulus, or seizures §, either:
|
First Occurrence of Grade 3 ICANS:
|
Recurrent Grade 3 ICANS:
|
||
| Grade 4 | ICE score 0 ‡, or depressed level of consciousness §: either:
|
|
| Adverse Reactions | Severity | Actions |
|---|---|---|
| Infections * | All Grades |
|
| Grade 3 |
|
|
| Grade 4 |
|
|
| Hematologic Toxicities | Absolute neutrophil count less than 0.5 × 10 9/L |
|
| Febrile neutropenia |
|
|
| Hemoglobin less than 8 g/dL |
|
|
| Platelet count less than 25,000/mcL Platelet count between 25,000/mcL and 50,000/mcL with bleeding |
|
|
| Other Non-Hematologic Adverse Reactions * |
Grade 3 |
|
| Grade 4 |
|
|
Preparation and Administration
TECVAYLI is intended for subcutaneous use by a healthcare provider only.
TECVAYLI should be administered by a healthcare provider with adequate medical personnel and appropriate medical equipment to manage severe reactions, including CRS and ICANS .
TECVAYLI is a clear to slightly opalescent, colorless to light yellow solution. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if the solution is discolored, or cloudy, or if foreign particles are present.
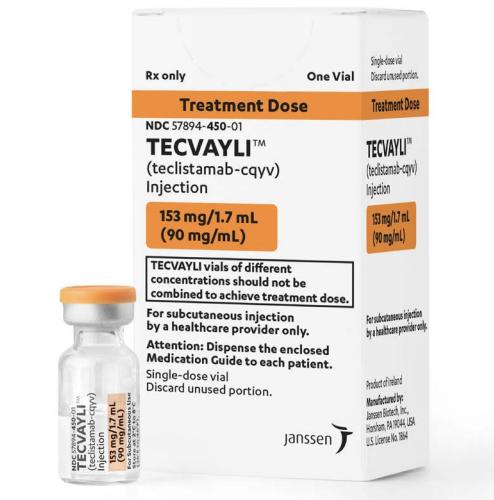
TECVAYLI 30 mg/3 mL (10 mg/mL) vial and TECVAYLI 153 mg/1.7 mL (90 mg/mL) vial are supplied as ready-to-use solution that do not need dilution prior to administration.
Do not combine TECVAYLI vials of different concentrations to achieve treatment dose.
Use aseptic technique to prepare and administer TECVAYLI.
Preparation of TECVAYLI
Refer to the following reference tables for the preparation of TECVAYLI.
Refer to Tables 7, 8, and 9 below to determine the dosage based on predetermined weight ranges.
Use Table 7 to determine total dose, injection volume and number of vials required based on patient's actual body weight for step-up dose 1 using TECVAYLI 30 mg/3 mL (10 mg/mL) vial.
| Patient Body Weight (kg) |
Total Dose (mg) |
Volume of Injection (mL) |
Number of Vials (1 vial=3 mL) |
|---|---|---|---|
| 35 to 39 | 2.2 | 0.22 | 1 |
| 40 to 44 | 2.5 | 0.25 | 1 |
| 45 to 49 | 2.8 | 0.28 | 1 |
| 50 to 59 | 3.3 | 0.33 | 1 |
| 60 to 69 | 3.9 | 0.39 | 1 |
| 70 to 79 | 4.5 | 0.45 | 1 |
| 80 to 89 | 5.1 | 0.51 | 1 |
| 90 to 99 | 5.7 | 0.57 | 1 |
| 100 to 109 | 6.3 | 0.63 | 1 |
| 110 to 119 | 6.9 | 0.69 | 1 |
| 120 to 129 | 7.5 | 0.75 | 1 |
| 130 to 139 | 8.1 | 0.81 | 1 |
| 140 to 149 | 8.7 | 0.87 | 1 |
| 150 to 160 | 9.3 | 0.93 | 1 |
Use Table 8 to determine total dose, injection volume and number of vials required based on patient's actual body weight for step-up dose 2 using TECVAYLI 30 mg/3 mL (10 mg/mL) vial.
| Patient Body Weight (kg) |
Total Dose (mg) |
Volume of Injection (mL) |
Number of Vials (1 vial=3 mL) |
|---|---|---|---|
| 35 to 39 | 11 | 1.1 | 1 |
| 40 to 44 | 13 | 1.3 | 1 |
| 45 to 49 | 14 | 1.4 | 1 |
| 50 to 59 | 16 | 1.6 | 1 |
| 60 to 69 | 19 | 1.9 | 1 |
| 70 to 79 | 22 | 2.2 | 1 |
| 80 to 89 | 25 | 2.5 | 1 |
| 90 to 99 | 28 | 2.8 | 1 |
| 100 to 109 | 31 | 3.1 | 2 |
| 110 to 119 | 34 | 3.4 | 2 |
| 120 to 129 | 37 | 3.7 | 2 |
| 130 to 139 | 40 | 4 | 2 |
| 140 to 149 | 43 | 4.3 | 2 |
| 150 to 160 | 47 | 4.7 | 2 |
Use Table 9 to determine total dose, injection volume and number of vials required based on patient's actual body weight for the treatment dose using TECVAYLI 153 mg/1.7 mL (90 mg/mL) vial.
| Patient Body Weight (kg) |
Total Dose (mg) |
Volume of Injection (mL) |
Number of Vials (1 vial=1.7 mL) |
|---|---|---|---|
| 35 to 39 | 56 | 0.62 | 1 |
| 40 to 44 | 63 | 0.7 | 1 |
| 45 to 49 | 70 | 0.78 | 1 |
| 50 to 59 | 82 | 0.91 | 1 |
| 60 to 69 | 99 | 1.1 | 1 |
| 70 to 79 | 108 | 1.2 | 1 |
| 80 to 89 | 126 | 1.4 | 1 |
| 90 to 99 | 144 | 1.6 | 1 |
| 100 to 109 | 153 | 1.7 | 1 |
| 110 to 119 | 171 | 1.9 | 2 |
| 120 to 129 | 189 | 2.1 | 2 |
| 130 to 139 | 198 | 2.2 | 2 |
| 140 to 149 | 216 | 2.4 | 2 |
| 150 to 160 | 234 | 2.6 | 2 |
Remove the appropriate strength TECVAYLI vial from refrigerated storage [2°C to 8°C (36°F to 46°F)].
Once removed from refrigerated storage, equilibrate TECVAYLI to ambient temperature [15°C to 30°C (59°F to 86°F)] for at least 15 minutes. Do not warm TECVAYLI in any other way.
Once equilibrated, gently swirl the vial for approximately 10 seconds to mix. Do not shake.
Withdraw the required injection volume of TECVAYLI from the vial(s) into an appropriately sized syringe using a transfer needle.
Each injection volume should not exceed 2 mL. Divide doses requiring greater than 2 mL equally into multiple syringes.
TECVAYLI is compatible with stainless steel injection needles and polypropylene or polycarbonate syringe material.
Replace the transfer needle with an appropriately sized needle for injection.
Administration of TECVAYLI
Inject the required volume of TECVAYLI into the subcutaneous tissue of the abdomen (preferred injection site). Alternatively, TECVAYLI may be injected into the subcutaneous tissue at other sites (e.g., thigh). If multiple injections are required, TECVAYLI injections should be at least 2 cm apart.
Do not inject into tattoos or scars or areas where the skin is red, bruised, tender, hard or not intact.
Any unused product or waste material should be disposed in accordance with local requirements.
Frequently asked questions
- What should I know about the Tecvayli REMS program?
- What is the mechanism of action for Tecvayli (teclistamab-cqyv)?
- What’s the difference between Tecvayli and Talvey?
- Is Tecvayli FDA approved as a multiple myeloma treatment?
- Where can I find the Tecvayli FDA package insert?
- What is the success rate of Tecvayli?
More about Tecvayli (teclistamab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Side effects
- During pregnancy
- FDA approval history
- Drug class: bispecific T-cell engagers (BiTE)
- Breastfeeding
- En español
Patient resources
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.