Metoclopramide Dosage
Medically reviewed by Drugs.com. Last updated on Aug 9, 2023.
Applies to the following strengths: 10 mg; 5 mg; 5 mg/5 mL; 5 mg/mL; 10 mg/mL; 15 mg/actuation
Usual Adult Dose for:
- Nausea/Vomiting - Chemotherapy Induced
- Nausea/Vomiting - Postoperative
- Small Intestine Intubation
- Radiographic Exam
- Gastroparesis
- Gastroesophageal Reflux Disease
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Nausea/Vomiting - Chemotherapy Induced
EMETOGENIC CANCER CHEMOTHERAPY:
Parenteral:
- Initial dose: 1 to 2 mg/kg/dose (depending on the emetogenic potential of the agent) IV infused over a period of not less than 15 minutes, 30 minutes before administration of chemotherapy.
- Subsequent doses: The dose should be repeated every 2 hours for 2 doses following the initial dose, then every 3 hours for 3 additional doses.
Comments:
- The initial 2 doses should be given at 2 mg/kg with highly emetogenic chemotherapy regimens and 1 mg/kg with less emetogenic regimens.
- For doses higher than 10 mg, the injection should be diluted in 50 mL of a parenteral solution. Normal saline is the preferred diluent.
- If acute dystonic reactions occur, 50 mg of diphenhydramine may be injected IM.
POSTOPERATIVE NAUSEA AND VOMITING:
Parenteral: 10 to 20 mg IM at or near the end of surgery
Uses:
- For the prophylaxis of nausea and vomiting associated with emetogenic cancer chemotherapy
- For the prophylaxis of postoperative nausea and vomiting where nasogastric suction is undesirable
Usual Adult Dose for Nausea/Vomiting - Postoperative
EMETOGENIC CANCER CHEMOTHERAPY:
Parenteral:
- Initial dose: 1 to 2 mg/kg/dose (depending on the emetogenic potential of the agent) IV infused over a period of not less than 15 minutes, 30 minutes before administration of chemotherapy.
- Subsequent doses: The dose should be repeated every 2 hours for 2 doses following the initial dose, then every 3 hours for 3 additional doses.
Comments:
- The initial 2 doses should be given at 2 mg/kg with highly emetogenic chemotherapy regimens and 1 mg/kg with less emetogenic regimens.
- For doses higher than 10 mg, the injection should be diluted in 50 mL of a parenteral solution. Normal saline is the preferred diluent.
- If acute dystonic reactions occur, 50 mg of diphenhydramine may be injected IM.
POSTOPERATIVE NAUSEA AND VOMITING:
Parenteral: 10 to 20 mg IM at or near the end of surgery
Uses:
- For the prophylaxis of nausea and vomiting associated with emetogenic cancer chemotherapy
- For the prophylaxis of postoperative nausea and vomiting where nasogastric suction is undesirable
Usual Adult Dose for Small Intestine Intubation
If the tube has not passed the pylorus with conventional maneuvers in 10 minutes, a single undiluted dose may be administered via slow IV.
Parenteral: 10 mg IV metoclopramide base over a 1- to 2-minute period
Use: To facilitate small bowel intubation in patients in whom the tube does not pass the pylorus with conventional measures
Usual Adult Dose for Radiographic Exam
In patients where delayed gastric emptying interferes with radiological examination of the stomach and/or small intestine, a single IV dose may be administered.
Parenteral: 10 mg IV metoclopramide base over a 1 to 2-minute period
Use: Stimulate gastric emptying and intestinal transit of barium in cases where delayed emptying interferes with radiological examination of the stomach and/or small intestine
Usual Adult Dose for Gastroparesis
Parenteral: 10 mg IV (slowly over a 1 to 2-minute period) or IM
- Maximum duration of therapy: Up to 10 days
Oral: 10 mg orally 30 minutes before each meal and at bedtime for 2 to 8 weeks, depending upon response and the likelihood of continued well-being upon drug discontinuation
- Maximum dose: 40 mg/day
- Maximum duration of therapy: 12 weeks
Comments:
- Oral administration may be initiated in the earliest manifestations of diabetic gastric stasis.
- IM/IV administration for up to 10 days if severe symptoms are present; once symptoms subside, the patient may be switched to oral therapy.
- Geriatric patients and those who are more sensitive to adverse effects may require an oral dose of 5 mg.
- Since diabetic gastric stasis is often recurrent, therapy should be reinstituted at the earliest manifestation.
Use: For the relief of symptoms associated with acute and recurrent diabetic gastric stasis/gastroparesis
Usual Adult Dose for Gastroesophageal Reflux Disease
Oral:
- Symptomatic gastroesophageal reflux disease (GERD): 10 to 15 mg orally up to 4 times a day (30 minutes before meals and at bedtime), depending upon symptoms being treated and clinical response
- Intermittent symptoms/at specific times of day: 20 mg orally once a day prior to provoking situation
- Use with esophageal erosions/ulcerations: 15 mg orally 4 times a day, if tolerated
- Maximum dose: 60 mg/day
- Maximum duration of therapy: 12 weeks
Comments:
- Geriatric patients and those who are more sensitive to adverse effects may require an oral dose of 5 mg.
- Because of the poor correlation between symptoms and endoscopic appearance of the esophagus, therapy directed at esophageal lesions is best guided by endoscopic evaluation.
Use: For the relief of symptomatic GERD in patients who fail to respond to conventional therapy
Usual Pediatric Dose for Small Intestine Intubation
If the tube has not passed the pylorus with conventional maneuvers in 10 minutes, a single undiluted dose may be administered via slow IV.
Parenteral:
6 years or younger: 0.1 mg/kg metoclopramide base IV over a 1 to 2 minute period
6 to 14 years: 2.5 to 5 mg metoclopramide base IV over a 1 to 2 minute period
14 years or older: 10 mg metoclopramide base IV over a 1 to 2 minute period
Comment: A single dose IV may be used if delayed gastric emptying interferes with radiological examination of the stomach and/or small intestine.
Uses:
- To facilitate small bowel intubation in patients in whom the tube does not pass the pylorus with conventional measures
- Stimulate gastric emptying and intestinal transit of barium in cases where delayed emptying interferes with radiological examination of the stomach and/or small intestine
Renal Dose Adjustments
Parenteral and oral dissolving tablets:
CrCl 40 mL/min or greater: No adjustment recommended
CrCl less than 40 mL/min: Initial doses should be 50% of the usual recommended dose; subsequent dose adjustments should be made according to patient response and tolerability.
Oral tablets:
DIABETIC GASTROPARESIS:
Mild renal dysfunction (CrCl 60 mL/min or greater): No adjustment recommended
Moderate to severe renal dysfunction (CrCl less than 60 mL/min): 5 mg orally 4 times a day (30 minutes before each meal and at bedtime)
- Maximum dose: 20 mg/day
- Maximum dose: 20 mg/day
GERD:
Mild renal dysfunction (CrCl 60 mL/min or greater): No adjustment recommended
Moderate to severe renal dysfunction (CrCl less than 60 mL/min): 5 mg orally 4 times a day (30 minutes before each meal and at bedtime)
- Maximum dose: 20 mg/day
- Maximum dose: 10 mg/day
Liver Dose Adjustments
Parenteral and oral dissolving tablets: No adjustment recommended.
Oral tablets:
DIABETIC GASTROPARESIS:
Mild liver dysfunction (Child-Pugh A): 10 mg orally 4 times a day (30 minutes before each meal and at bedtime)
- Maximum dose: 40 mg/day
- Maximum dose: 20 mg/day
GERD:
Mild liver dysfunction (Child-Pugh A): 10 to 15 mg orally 4 times a day (30 minutes before each meal and at bedtime)
- Maximum dose: 60 mg/day
- Maximum dose: 30 mg/day
Dose Adjustments
Parenteral and oral dissolving tablets:
- The elderly may be more susceptible to developing adverse effects due to the changes in organ function, concomitant diseases, and other drug therapies.
- Patients with a higher sensitivity to adverse events (e.g., geriatric patients) may need 5 mg doses to treat symptomatic GERD.
- When used for the treatment of nausea and vomiting due to cytotoxic drug therapy, doses should be adjusted according to the emetogenicity of the cytotoxic drug.
Oral tablets:
CYP450 2D6 poor metabolizers OR use with strong CYP450 2D6 inhibitors:
DIABETIC GASTROPARESIS: 5 mg orally 4 times a day (30 minutes before each meal and at bedtime)
- Maximum dose: 20 mg/day
GERD: 5 mg orally 4 times a day (30 minutes before each meal and at bedtime) OR 10 mg orally 3 times a day
- Maximum dose: 30 mg/day
Precautions
US BOXED WARNINGS:
TARDIVE DYSKINESIA:
- Treatment with this drug can cause tardive dyskinesia, a serious movement disorder that is often irreversible. The risk of developing tardive dyskinesia increases with the duration of treatment and the total cumulative dose.
- This drug should be discontinued in patients who develop signs/symptoms of tardive dyskinesia. There is no known treatment for tardive dyskinesia. In some patients, symptoms may lessen or resolve after treatment is stopped.
- Treatment with this drug for longer than 12 weeks should be avoided in all but rare cases where therapeutic benefit is thought to outweigh the risk of developing tardive dyskinesia.
- Some manufacturers recommend: Avoid treatment with this drug for longer than 12 weeks because of the increased risk of developing tardive dyskinesia with longer-term use.
Safety and effectiveness of oral formulations (e.g., tablets, disintegrating tablets, solution) have not been established in pediatric patients (less than 18 years of age).
Safety and effectiveness of injection formulations have not been established in pediatric patients (less than 18 years of age) except to facilitate small bowel intubation.
Consult WARNINGS section for additional precautions.
Dialysis
US/CA:
Parenteral and oral dissolving tablets: Data not available
Oral tablets:
DIABETIC GASTROPARESIS:
Hemodialysis or continuous ambulatory peritoneal dialysis: 5 mg orally 4 times a day (30 minutes before each meal and at bedtime) OR 10 mg orally 2 times a day
- Maximum dose: 20 mg/day
GERD:
Hemodialysis or continuous ambulatory peritoneal dialysis: 5 mg orally 2 times a day
- Maximum dose: 10 mg/day
Other Comments
Administration advice:
- Therapy should not exceed 5 days (AU, UK) or 12 weeks (US) in duration.
- Dosage recommendations given should be strictly followed to avoid dystonic side effects.
- A minimum interval of 6 hours between administrations should be followed, even in cases of vomiting or rejection of the dose.
- Oral formulations should be taken on an empty stomach at least 30 minutes before eating since food can decrease the peak concentrations of drug in the bloodstream and/or the time it takes to achieve the maximum drug level in the bloodstream. If this drug is inadvertently taken with food, do not repeat the dose.
- Since the orally disintegrating tablet absorbs moisture rapidly, each dose should only be removed from the packaging just prior to taking. The tablet should be handled with dry hands and placed on the tongue. If the tablet breaks or crumbles while handling, it should be discarded and a new tablet should be removed. The tablet disintegrates on the tongue in approximately one minute and need not be taken with liquid.
- Parenteral formulations should be inspected for particulate matter and/or discoloration before administration. IV injections should be given slowly over at least 1 to 2 minutes. IV infusions should be diluted in at least 50 mL of suitable diluent and administered over at least 15 minutes.
Reconstitution/preparation techniques:
- The manufacturer product information should be consulted.
Storage requirements:
- The manufacturer product information should be consulted.
General:
- There is no clear benefit in motion sickness or other labyrinth disturbances.
- Extrapyramidal disorders may occur, particularly in children and young adults and/or when high doses are used.
- All patients on prolonged treatment should be reassessed regularly. Patients receiving this drug for disorders associated with delayed gastric emptying should be reviewed at an early stage for response to treatment.
- If vomiting persists, the patient should be reassessed to exclude the possibility of an underlying disorder, (i.e. cerebral irritation).
- Concomitant use with oral analgesics may improve analgesic absorption in the treatment of acute migraines.
- Use in patients 1 to 20 years old should be limited to severe intractable vomiting of known cause, vomiting associated with radiotherapy and intolerance to cytotoxic drugs, and as an aid to gastrointestinal intubation as part of surgical premedication.
Patient advice:
- Patients should be instructed to read the medication guide dispensed with their prescription initially and with each refill.
- Patients should be told to immediately report any signs/symptoms of tardive dyskinesia, neuroleptic malignant syndrome, or extrapyramidal symptoms; patients should consult with their healthcare provider if vomiting persists while on treatment.
- Patients should be advised that this drug may cause drowsiness, dizziness, dyskinesia and dystonia. Alcohol may increase the severity of these symptoms. Affected patients should avoid driving or using machinery until the full effects of this drug are known.
- Advise patients to speak to their healthcare provider if they become pregnant, intend to become pregnant, or are breastfeeding.
- Tell patients to report all concurrent prescription and nonprescription medications or herbal products they are taking.
More about metoclopramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (514)
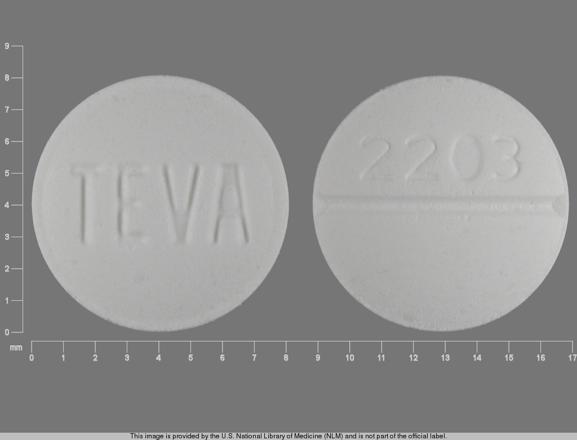
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Drug class: GI stimulants
- Breastfeeding
Patient resources
- Metoclopramide drug information
- Metoclopramide nasal
- Metoclopramide (Injection, Intravenous) (Advanced Reading)
- Metoclopramide Orally Disintegrating Tablets
Other brands
Professional resources
- Metoclopramide monograph
- Metoclopramide Injection (FDA)
- Metoclopramide Oral Solution (FDA)
- Metoclopramide Orally DisintegratingTablets (FDA)
- Metoclopramide Tablets (FDA)
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.