Atezolizumab Dosage
Medically reviewed by Drugs.com. Last updated on Feb 7, 2024.
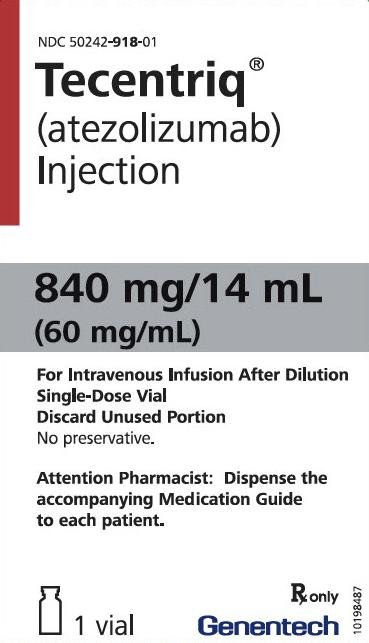
Applies to the following strengths: 1200 mg/20 mL; 840 mg/14 mL
Usual Adult Dose for:
- Urothelial Carcinoma
- Non-Small Cell Lung Cancer
- Breast Cancer
- Small Cell Lung Cancer
- Hepatocellular Carcinoma
- Melanoma - Metastatic
Additional dosage information:
Usual Adult Dose for Urothelial Carcinoma
MONOTHERAPY:
840 mg IV every 2 weeks OR 1200 mg IV every 3 weeks OR 1680 mg IV every 4 weeks until disease progression or unacceptable toxicity
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
Comments:
- Select cisplatin-ineligible patients with previously untreated locally advanced or metastatic UC for therapy with this drug based on the PD-L1 expression on tumor-infiltrating immune cells.
Use: For patients with locally advanced or metastatic urothelial carcinoma (UC) who are not eligible for cisplatin-containing chemotherapy and whose tumors express PD-L1 (PD-L1 stained tumor-infiltrating immune cells [IC] covering 5% or greater of the tumor area) OR are not eligible for any platinum-containing chemotherapy regardless of level of tumor PD-L1 expression OR have disease progression during or following any platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant chemotherapy.
Usual Adult Dose for Non-Small Cell Lung Cancer
MONOTHERAPY:
840 mg IV every 2 weeks OR 1200 mg IV every 3 weeks OR 1680 mg IV every 4 weeks until disease progression or unacceptable toxicity
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
IN COMBINATION WITH PLATINUM-BASED CHEMOTHERAPY:
1200 mg IV every 3 weeks until disease progression or unacceptable toxicity; administer atezolizumab prior to chemotherapy and bevacizumab when given on the same day; following completion of 4 to 6 cycles of chemotherapy, and if bevacizumab is discontinued, the recommended dosage of atezolizumab is:
840 mg IV every 2 weeks OR 1200 mg IV every 3 weeks OR 1680 mg IV every 4 weeks until disease progression or unacceptable toxicity
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
Comments:
- When administering this drug in combination with chemotherapy or other antineoplastic drugs, administer this drug prior to chemotherapy or other antineoplastic drugs when given on the same day.
- Refer to the Prescribing Information for bevacizumab, paclitaxel, and carboplatin for recommended dosing information.
Uses:
Non-small cell lung cancer (NSCLC):
- As a single agent for first-line treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) whose tumors have high PD-L1 expression (PD-L1 stained 50% or greater of tumor cells or PD-L1 stained tumor-infiltrating immune cells covering 10% or greater of the tumor area.
- In combination with bevacizumab, paclitaxel, and carboplatin, for first-line treatment of adult patients with metastatic non-squamous NSCLC with no EGFR or ALK genomic tumor aberrations.
- In combination with paclitaxel protein-bound and carboplatin, for first-line treatment of adult patients with metastatic non-squamous NSCLC with no EGFR or ALK genomic tumor aberrations.
- As a single-agent, for the treatment of adult patients with metastatic NSCLC who have disease progression during or following platinum-containing chemotherapy (patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for NSCLC harboring these aberrations prior to receiving this drug).
Usual Adult Dose for Breast Cancer
840 mg IV on Days 1 and 15 followed by paclitaxel protein-bound 100 mg/m2 IV on Days 1, 8, and 15 for each 28-day cycle until disease progression or unacceptable toxicity
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
Comments:
- Atezolizumab and paclitaxel protein-bound may be discontinued for toxicity independently of each other.
- Refer to the Prescribing Information for paclitaxel protein-bound for recommended dosing information.
- Do not substitute paclitaxel protein-bound with paclitaxel in combination with atezolizumab in clinical practice for metastatic TNBC outside of controlled trials.
Use:
Triple-Negative Breast Cancer (TNBC): In combination with paclitaxel protein-bound for the treatment of adult patients with unresectable locally advanced or metastatic TNBC whose tumors express PD-L1 (PD-L1 stained tumor-infiltrating immune cells [IC] of any intensity covering 1% or greater of the tumor area), as determined by an approved test (this drug is not indicated for use in combination with paclitaxel for the treatment of adult patients with unresectable locally advanced or metastatic TNBC).
Usual Adult Dose for Small Cell Lung Cancer
1200 mg IV every 3 weeks in combination with carboplatin and etoposide until disease progression or unacceptable toxicity; following completion of 4 cycles of carboplatin and etoposide, the recommended dosage of atezolizumab is:
840 mg IV every 2 weeks OR 1200 mg IV every 3 weeks OR 1680 mg IV every 4 weeks until disease progression or unacceptable toxicity
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
Comments:
- When administering atezolizumab in combination with chemotherapy, administer it prior to chemotherapy when given on the same day.
- Refer to the prescribing information for the chemotherapy agents administered in combination with this drug for recommended dosing information.
Use: In combination with carboplatin and etoposide for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC)
Usual Adult Dose for Hepatocellular Carcinoma
1200 mg IV over 60 minutes, followed by 15 mg/kg of bevacizumab on the same day, every 3 weeks until disease progression or unacceptable toxicity; if bevacizumab is discontinued for toxicity, the recommended dosage of atezolizumab is:
840 mg IV over 60 minutes every 2 weeks
OR
1200 mg IV over 60 minutes every 3 weeks
OR
1680 mg IV over 60 minutes every 4 weeks
Duration of therapy: Until disease progression or unacceptable toxicity.
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
Comments:
- Refer to the Prescribing Information for bevacizumab prior to initiation.
Use: In combination with bevacizumab for the treatment of patients with unresectable or metastatic hepatocellular carcinoma (HCC) who have not received prior systemic therapy
Usual Adult Dose for Melanoma - Metastatic
Prior to initiating atezolizumab, patients should receive a 28 day treatment cycle of cobimetinib 60 mg orally once a day (21 days on and 7 days off) and vemurafenib 960 mg orally 2 times a day on Days 1 through 21, and vemurafenib 720 mg orally 2 times a day on Days 22 through 28.
Atezolizumab dose: 840 mg IV over 60 minutes every 2 weeks until disease progression or unacceptable toxicity, when administered with cobimetinib 60 mg orally once a day (21 days on and 7 days off) and vemurafenib 720 mg orally 2 times a day
NOTE: Administer the first infusion over 60 minutes; if well tolerated, administer subsequent infusions over 30 minutes
Comments:
- Refer to the Prescribing Information for cobimetinib and vemurafenib prior to initiation.
Use: In combination with cobimetinib and vemurafenib for the treatment of patients with BRAF V600 mutation-positive unresectable or metastatic melanoma
Renal Dose Adjustments
Mild to moderate renal impairment: No adjustment recommended.
Severe renal impairment: Data not available
THERAPY MODIFICATIONS FOR ADVERSE REACTIONS:
NEPHRITIS WITH RENAL DYSFUNCTION:
- Grades 2 or 3 increased blood creatinine: Withhold therapy; resume with complete or partial resolution (Grade 0 to 1) after corticosteroid taper; permanently discontinue if no complete or partial resolution within 12 weeks of initiating steroids or inability to reduce prednisone to 10 mg per day or less (or equivalent) within 12 weeks of initiating steroids.
- Grade 4 increased blood creatinine: Permanently discontinue therapy.
Liver Dose Adjustments
Mild hepatic impairment: No adjustment recommended.
Moderate to severe hepatic impairment: Data not available
THERAPY MODIFICATIONS FOR ADVERSE REACTIONS:
HEPATITIS WITH NO TUMOR INVOLVEMENT OF THE LIVER:
- ALT or AST greater than 3 and up to 8 times upper limit of normal [ULN] or total blood bilirubin greater than 1.5 and up to 3 x ULN: Withhold therapy until Grade 1 or resolved and corticosteroid dose is less than or equal to prednisone 10 mg per day (or equivalent).
- ALT or AST greater than 8 x ULN or blood bilirubin greater than 3 x ULN: Permanently discontinue therapy.
- Baseline AST or ALT is more than 1 and up to 3 times upper limit of normal (ULN) and increases to more than 5 and up to 10 x ULN or baseline AST or ALT is more than 3 and up to 5 x ULN and increases to more than 8 and up to 10 x ULN: Withhold therapy; resume with complete or partial resolution (Grade 0 to 1) after corticosteroid taper; permanently discontinue if no complete or partial resolution within 12 weeks of initiating steroids or inability to reduce prednisone to 10 mg per day or less (or equivalent) within 12 weeks of initiating steroids.
- If AST or ALT increases to more than 10 x ULN or total bilirubin increases to more than 3 x ULN: Permanently discontinue therapy.
Dose Adjustments
Dose Modifications: No dose reductions of this drug are recommended. In general, withhold therapy for severe (Grade 3) immune-mediated adverse reactions. Permanently discontinue therapy for life-threatening (Grade 4) immune-mediated adverse reactions, recurrent severe (Grade 3) immune-mediated reactions that require systemic immunosuppressive treatment, or an inability to reduce corticosteroid dose to 10 mg or less of prednisone or equivalent per day within 12 weeks of initiating steroids.
THERAPY MODIFICATIONS FOR ADVERSE REACTIONS:
PNEUMONITIS:
- Grade 2: Withhold therapy; resume with complete or partial resolution (Grade 0 to 1) after corticosteroid taper; permanently discontinue if no complete or partial resolution within 12 weeks of initiating steroids or inability to reduce prednisone to 10 mg per day or less (or equivalent) within 12 weeks of initiating steroids. when the event improves to Grade 1 or resolved, and corticosteroids have been reduced to 10 mg or less oral prednisone or equivalent per day.
- Grade 3 or 4: Permanently discontinue therapy.
- Grade 2 or 3: Withhold therapy; resume with complete or partial resolution (Grade 0 to 1) after corticosteroid taper; permanently discontinue if no complete or partial resolution within 12 weeks of initiating steroids or inability to reduce prednisone to 10 mg per day or less (or equivalent) within 12 weeks of initiating steroids.
- Grade 4: Permanently discontinue therapy.
- Grade 3 or 4: Withhold dose until stable or permanently discontinue depending on severity.:
- Suspected Stevens Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), or Drug Rash with Eosinophilia and Systemic Symptoms (DRESS): Withhold therapy; resume with complete or partial resolution (Grade 0 to 1) after corticosteroid taper; permanently discontinue if no complete or partial resolution within 12 weeks of initiating steroids or inability to reduce prednisone to 10 mg per day or less (or equivalent) within 12 weeks of initiating steroids. when the event improves to Grade 1 or resolved, and corticosteroids have been reduced to 10 mg or less oral prednisone or equivalent per day.
- Confirmed SJS, TEN, or DRESS: Permanently discontinue therapy.
- Grades 2, 3, or 4: Permanently discontinue therapy.
- Grade 2: Withhold therapy; resume with complete or partial resolution (Grade 0 to 1) after corticosteroid taper; permanently discontinue if no complete or partial resolution within 12 weeks of initiating steroids or inability to reduce prednisone to 10 mg per day or less (or equivalent) within 12 weeks of initiating steroids. when the event improves to Grade 1 or resolved, and corticosteroids have been reduced to 10 mg or less oral prednisone or equivalent per day.
- Grades 3 or 4: Permanently discontinue therapy.
- Grade 1 or 2: Interrupt or slow the rate of infusion.
- Grade 3 or 4: Permanently discontinue therapy.
Precautions
CONTRAINDICATIONS:
- None
Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Administer the initial infusion over 60 minutes through an IV line with or without a sterile, non-pyrogenic, low-protein binding in-line filter (pore size of 0.2 to 0.22 micron).
- If the first infusion is tolerated, all subsequent infusions may be delivered over 30 minutes.
- If a dose is missed, it should be administered as soon as possible; do not wait until the next dose.
- Do not administer this drug as an IV push or bolus.
- Do not coadminister other drugs through the same IV line.
Storage requirements:
- Store in a refrigerator (2C to 8C).
- Do not freeze.
- Keep the vial in the outer carton to protect from light.
- Administer immediately when prepared as this product does not contain a preservative.
- If the diluted solution is not used immediately, store solution either at room temperature for no more than 6 hours from time of preparation including room temperature storage of the infusion in the infusion bag and time for administration of the infusion OR store under refrigeration at 2C to 8C (36F to 46F) for no more than 24 hours from time of preparation. Do not freeze. Do not shake.
General:
- To improve the traceability of biological medicinal products, the trade name and the batch number of the administered product should be recorded in the patient medical record.
Frequently asked questions
- Are there cost-saving programs for Tecentriq?
- How effective is it?
- Is atezolizumab (Tecentriq) a chemotherapy or immunotherapy drug?
- Does atezolizumab (Tecentriq) cause hair loss?
- How is atezolizumab (Tecentriq) administered?
- What type of cancer is Tecentriq used to treat?
More about atezolizumab
- Check interactions
- Compare alternatives
- Reviews (6)
- Latest FDA alerts (2)
- Side effects
- During pregnancy
- Drug class: anti-PD-1 and PD-L1 monoclonal antibodies (immune checkpoint inhibitors)
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.