Alvaiz Dosage
Generic name: ELTROMBOPAG CHOLINE 9mg
Dosage form: tablet, film coated
Drug class: Platelet-stimulating agents
Medically reviewed by Drugs.com. Last updated on Feb 13, 2024.
Important Dosage Information
- Eltrombopag is available for different indications and in different dosage forms and tablet strengths.
- ALVAIZ is not substitutable with other eltrombopag products on a milligram per milligram basis due to the observed bioavailability in studies conducted on ALVAIZ.
- Patients must be able to swallow ALVAIZ tablets whole [see Dosage and Administration (2.5)].
Recommended Dosage for Persistent or Chronic Immune Thrombocytopenia
Use the lowest dose of ALVAIZ to achieve and maintain a platelet count greater than or equal to 50 x 109/L as necessary to reduce the risk for bleeding. Dose adjustments are based upon the platelet count response. Do not use ALVAIZ to normalize platelet counts [see Warnings and Precautions (5.4)]. In clinical trials, platelet counts generally increased within 1 to 2 weeks after starting ALVAIZ and decreased within 1 to 2 weeks after discontinuing ALVAIZ [see Clinical Studies (14.1)].
Initial Dose Regimen: Adult and Pediatric Patients 6 Years and Older with ITP: Initiate ALVAIZ at a dose of 36 mg orally once daily, except in patients who are of East-/Southeast-Asian ancestry or who have mild to severe hepatic impairment (Child-Pugh Class A, B, C).
For patients of East-/Southeast-Asian ancestry with ITP, initiate ALVAIZ at a reduced dose of 18 mg once daily [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)].
For patients with ITP and mild, moderate, or severe hepatic impairment (Child-Pugh Class A, B, C), initiate ALVAIZ at a reduced dose of 18 mg once daily [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
For patients of East-/Southeast-Asian ancestry with ITP and hepatic impairment (Child-Pugh Class A, B, C), consider initiating ALVAIZ at a reduced dose of 9 mg once daily [see Clinical Pharmacology (12.3)].
Monitoring and Dose Adjustment: After initiating ALVAIZ, adjust the dose to achieve and maintain a platelet count greater than or equal to 50 x 109/L as necessary to reduce the risk for bleeding. Do not exceed a dose of 54 mg daily. Monitor clinical hematology and liver tests regularly throughout therapy with ALVAIZ and modify the dosage regimen of ALVAIZ based on platelet counts as outlined in Table 1. During therapy with ALVAIZ, assess complete blood counts (CBCs) with differentials, including platelet counts, weekly until a stable platelet count has been achieved. Obtain CBCs with differentials, including platelet counts, monthly thereafter.
|
Platelet Count Result |
Dose Adjustment or Response |
|
< 50 x 109/L following at least 2 weeks of ALVAIZ |
Increase daily dose by 18 mg to a maximum of 54 mg/day. For patients taking 9 mg once daily, increase the dose to 18 mg daily before increasing the dose amount by 18 mg. |
|
≥ 200 x 109/L to ≤ 400 x 109/L at any time |
Decrease the daily dose by 18 mg. Wait 2 weeks to assess the effects of this and any subsequent dose adjustments. For patients taking 18 mg once daily, decrease the dose to 9 mg once daily. |
|
> 400 x 109/L |
Stop ALVAIZ; increase the frequency of platelet monitoring to twice weekly. Once the platelet count is < 150 x 109/L, reinitiate therapy at a daily dose reduced by 18 mg. For patients taking 18 mg once daily, reinitiate therapy at a daily dose of 9 mg. |
|
> 400 x 109/L after 2 weeks of therapy at lowest dose of ALVAIZ |
Discontinue ALVAIZ. |
In patients with ITP and hepatic impairment (Child-Pugh Class A, B, C), after initiating ALVAIZ or after any subsequent dosing increase, wait 3 weeks before increasing the dose.
Modify the dosage regimen of concomitant ITP medications, as medically appropriate, to avoid excessive increases in platelet counts during therapy with ALVAIZ. Do not administer more than one dose of ALVAIZ within any 24-hour period.
Discontinuation: Discontinue ALVAIZ if the platelet count does not increase to a level sufficient to avoid clinically important bleeding after 4 weeks of therapy with ALVAIZ at the maximum daily dose of 54 mg. Excessive platelet count responses, as outlined in Table 1, or important liver test abnormalities also necessitate discontinuation of ALVAIZ [see Warnings and Precautions (5.2)]. Obtain CBCs with differentials, including platelet counts, weekly for at least 4 weeks following discontinuation of ALVAIZ.
Recommended Dosage for Chronic Hepatitis C-associated Thrombocytopenia
Use the lowest dose of ALVAIZ to achieve and maintain a platelet count necessary to initiate and maintain antiviral therapy with pegylated interferon and ribavirin. Dose adjustments are based upon the platelet count response. Do not use ALVAIZ to normalize platelet counts [see Warnings and Precautions (5.4)]. In clinical trials, platelet counts generally began to rise within the first week of treatment with ALVAIZ [see Clinical Studies (14.2)].
Initial Dose Regimen: Initiate ALVAIZ at a dose of 18 mg orally once daily.
Monitoring and Dose Adjustment: Adjust the dose of ALVAIZ in 18-mg increments every 2 weeks as necessary to achieve the target platelet count required to initiate antiviral therapy. Monitor platelet counts every week prior to starting antiviral therapy.
During antiviral therapy, adjust the dose of ALVAIZ to avoid dose reductions of peginterferon. Monitor CBCs with differentials, including platelet counts, weekly during antiviral therapy until a stable platelet count is achieved. Monitor platelet counts monthly thereafter. Do not exceed a dose of 72 mg daily. Monitor clinical hematology and liver tests regularly throughout therapy with ALVAIZ.
For specific dosage instructions for peginterferon or ribavirin, refer to their respective prescribing information.
|
Platelet Count Result |
Dose Adjustment or Response |
|
< 50 x 109/L following at least |
Increase daily dose by 18 mg to a maximum of 72 mg/day. |
|
≥ 200 x 109/L to ≤ 400 x 109/L at any time |
Decrease the daily dose by 18 mg. Wait 2 weeks to assess the effects of this and any subsequent dose adjustments. |
|
> 400 x 109/L |
Stop ALVAIZ; increase the frequency of platelet monitoring to twice weekly. Once the platelet count is < 150 x 109/L, reinitiate therapy at a daily dose reduced by 18 mg. For patients taking 18 mg once daily, reinitiate therapy at a daily dose of 9 mg. |
|
> 400 x 109/L after 2 weeks of therapy at lowest dose of ALVAIZ |
Discontinue ALVAIZ. |
Discontinuation: The prescribing information for pegylated interferon and ribavirin include recommendations for antiviral treatment discontinuation for treatment futility. Refer to pegylated interferon and ribavirin prescribing information for discontinuation recommendations for antiviral treatment futility.
ALVAIZ should be discontinued when antiviral therapy is discontinued. Excessive platelet count responses, as outlined in Table 2, or important liver test abnormalities also necessitate discontinuation of ALVAIZ [see Warnings and Precautions (5.2)].
Recommended Dosage for Refractory Severe Aplastic Anemia
Use the lowest dose of ALVAIZ to achieve and maintain a hematologic response. Dose adjustments are based upon the platelet count. Hematologic response requires dose titration, generally up to 108 mg, and may take up to 16 weeks after starting ALVAIZ [see Clinical Studies (14.3)].
Initial Dose Regimen: Initiate ALVAIZ at a dose of 36 mg orally once daily.
For patients with severe aplastic anemia of East-/Southeast-Asian ancestry or those with mild, moderate, or severe hepatic impairment (Child-Pugh Class A, B, C), initiate ALVAIZ at a reduced dose of 18 mg once daily [see Use in Specific Populations (8.6, 8.7), Clinical Pharmacology (12.3)].
Monitoring and Dose Adjustment: Adjust the dose of ALVAIZ in 36-mg increments every 2 weeks as necessary to achieve the target platelet count greater than or equal to 50 x 109/L as necessary. Do not exceed a dose of 108 mg daily. Monitor clinical hematology and liver tests regularly throughout therapy with ALVAIZ and modify the dosage regimen of ALVAIZ based on platelet counts as outlined in Table 3.
|
Platelet Count Result |
Dose Adjustment or Response |
|
< 50 x 109/L following at least |
Increase daily dose by 36 mg to a maximum of 108 mg/day. For patients taking 18 mg once daily, increase the dose to 36 mg daily before increasing the dose amount by 36 mg. |
|
≥ 200 x 109/L to ≤ 400 x 109/L |
Decrease the daily dose by 36 mg. Wait 2 weeks to assess the effects of this and any subsequent dose adjustments. |
|
> 400 x 109/L |
Stop ALVAIZ for 1 week. Once the platelet count is < 150 x 109/L, reinitiate therapy at a dose reduced by 36 mg. |
|
> 400 x 109/L after 2 weeks of therapy at lowest dose of ALVAIZ |
Discontinue ALVAIZ. |
For patients who achieve tri-lineage response, including transfusion independence, lasting at least 8 weeks: the dose of ALVAIZ may be reduced by 50% [see Clinical Studies (14.3)]. If counts remain stable after 8 weeks at the reduced dose, then discontinue ALVAIZ and monitor blood counts. If platelet counts drop to less than 30 x 109/L, hemoglobin to less than 9 g/dL, or absolute neutrophil count (ANC) to less than 0.5 x 109/L, ALVAIZ may be reinitiated at the previous effective dose.
Discontinuation: If no hematologic response has occurred after 16 weeks of therapy with ALVAIZ, discontinue therapy. If new cytogenetic abnormalities are observed, consider discontinuation of ALVAIZ [see Adverse Reactions (6.1)]. Excessive platelet count responses (as outlined in Table 3) or important liver test abnormalities also necessitate discontinuation of ALVAIZ [see Warnings and Precautions (5.2)].
Administration
Administration of Tablets: Take ALVAIZ without a meal or with a meal low in calcium (≤ 50 mg). Take ALVAIZ at least 2 hours before or 4 hours after other medications (e.g., antacids), calcium-rich foods (containing > 50 mg calcium e.g., dairy products, calcium-fortified juices, and certain fruits and vegetables), or supplements containing polyvalent cations, such as iron, calcium, aluminum, magnesium, selenium, and zinc [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
Swallow tablets whole. Do not split, chew, or crush tablets and mix with food or liquids.
More about Alvaiz (eltrombopag)
- Check interactions
- Compare alternatives
- Pricing & coupons
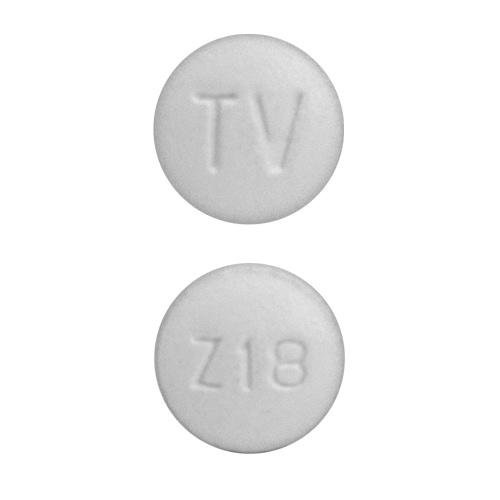
- Drug images
- Side effects
- During pregnancy
- FDA approval history
- Drug class: platelet-stimulating agents
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.