Below the Knee Amputation
Medically reviewed by Drugs.com. Last updated on Nov 3, 2024.
Below the knee amputation is surgery to remove your leg below your knee cap. You may need an amputation because of an injury, a tumor, or an infection. Problems with your leg veins or arteries, or complications of diabetes may also cause you to need an amputation. The part of your leg that is not removed is called a residual limb. You will be shown how to care for your residual limb. You can also work with specialists to have prosthetics made for you. A prosthetic will help you return to your normal daily activities.
DISCHARGE INSTRUCTIONS:
Seek care immediately if:
- You have severe pain in your residual limb.
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You suddenly feel lightheaded and have shortness of breath.
- You have chest pain. You may have more pain when you take a deep breath or cough. You may cough up blood.
- Your stitches come apart.
- Blood soaks through your bandage.
Contact your healthcare provider or orthopedist if:
- You have a fever.
- The skin around your stitches is red, swollen, or has pus coming from the wound.
- You have a sudden increase in tenderness in your residual limb.
- You have chills, a cough, or feel weak and achy.
- Your skin is itchy, swollen, or has a rash.
- You feel anxious, depressed, or have trouble coping with your condition.
- You have questions or concerns about your surgery or care.
Medicines:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Muscle relaxers help decrease pain and muscle spasms.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Follow up with your healthcare provider or orthopedist as directed:
You may have a home health care nurse help you between your visits. You may need to return to have your stitches removed. Write down your questions so you remember to ask them during your visits.
Physical and occupational therapy:
A physical therapist will help you with exercises to improve your strength. You may be fitted with a prosthesis, which may need to be adjusted several times before it fits well. Physical therapists will also help you learn to walk with the prosthesis and with crutches. Occupational therapists will help you adjust to daily activities at home and work.
Care for your residual limb:
- Clean and care for your skin. When you are allowed to bathe, gently wash around the incision with soap and water. It is okay to let soap and water run over your incision. Take showers instead of baths. Do not soak in a tub or hot tub, and do not swim. These could cause an infection. Your healthcare provider will tell you when it is okay to do these activities again. Carefully rinse and dry your skin. Look closely at the skin on your residual limb every day. Use a hand mirror to see all sides of your residual limb. Look for redness, blisters, or scrapes. Do not put lotion, oil, cream, or rubbing alcohol on your residual limb. Rubbing alcohol dries and cracks your skin.
- Prevent infection. Wash your hands before you touch your wound. This will help prevent an infection. Only use antiseptic (germ-killing) medicines if healthcare providers tell you to.
- Help your residual limb heal. Push the residual limb against a soft pillow. Slowly increase the pressure and start to push your residual limb against harder surfaces, such as the back of a chair. Massage the residual limb to soften the scar, decrease tenderness, and improve blood flow.
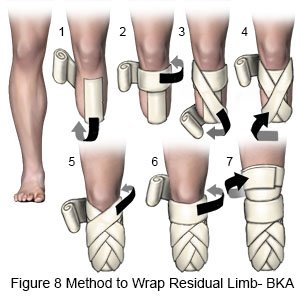
Wrap your residual limb:
Wrap your limb to help form it into a firm cone shape so it will fit a prosthesis. Keep the bandage on at all times except when you bathe. Rewrap the residual limb 2 to 3 times each day to keep the bandage smooth and tight. At first you will not pull the elastic bandage very tight. Healthcare providers will have you pull the bandage tighter as your wound heals and the stitches are removed. If your residual limb hurts or throbs, the bandage may be too tight. Unwrap your limb and start over. The following are directions for the figure of 8 method to wrap your residual limb:
- Hold the bandage roll on your thigh with one hand. Use the other hand to roll the bandage diagonally down your thigh. Stretch the bandage slightly when you get to the bottom of your limb. Wrap the bandage around the end of the limb.
- Roll the bandage around to the front. Continue diagonally up your thigh. The bandage will cross over itself. Roll the bandage all the way around the limb and to the front again.
- Repeat these steps until your limb is completely covered from mid-thigh down. Overlap the bandage as you wrap, so that you are always covering new skin. If you need to use more than one bandage, secure each bandage with a clip or tape before you apply the next.
- When you are finished, secure the last bandage. Try to end the bandage in a place that is not in a skin fold or at your knee joint.
-
Woolen residual limb socks:
Wear a woolen residual limb sock when healthcare providers say you no longer need to wrap your residual limb. This keeps your residual limb clean and comfortable. Wash the woolen socks gently in cool water and soap to keep them from shrinking. Dry the socks flat on a towel to prevent stretching. Replace the sock if it gets torn.
Activity:
- Slowly increase your activity level. Rest when needed, but try to exercise 2 to 3 times each day or as directed by your healthcare provider. Do not put weight on your residual limb until healthcare providers tell you it is okay. Many companies supply sports equipment for people with amputations. Talk to your healthcare provider if you are interested in getting a prosthesis so you can stay active in sports.
- Ask your healthcare provider when you can return to work or school. Ask when you can begin to drive.
For support and more information:
- Amputee Coalition
900 E. Hill Ave, Ste 290
Knoxville, , TN 37915
Phone: 1- 888 - 267-5669
Web Address: www.amputee-coalition.org
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
