Quinine Side Effects
Medically reviewed by Drugs.com. Last updated on Jan 13, 2024.
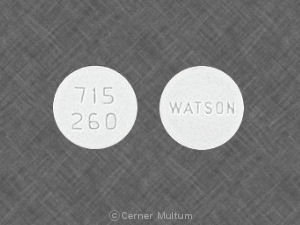
Applies to quinine: oral capsule.
Warning
Oral route (Capsule)
Quinine sulfate use for the treatment or prevention of nocturnal leg cramps may result in serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP). Chronic renal impairment associated with the development of TTP has been reported. The risk associated with quinine sulfate use in the absence of evidence of its effectiveness in the treatment or prevention of nocturnal leg cramps outweighs any potential benefit.
Serious side effects of Quinine
Along with its needed effects, quinine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking quinine:
More common
- Blurred vision
- change in color vision
- changes in behavior
- confusion
- diarrhea
- hearing loss
- nausea
- ringing in the ears
- stomach cramps or pain
- vomiting
Less common
- Anxiety
- behavior change, similar to drunkenness
- black, tarry stools
- bloody urine
- blurred vision or change in vision
- chills
- cold sweats
- confusion
- cool pale skin
- cough
- difficulty concentrating
- drowsiness
- excessive hunger
- fast heartbeat
- fever
- headache
- hoarseness
- loss of consciousness
- lower back or side pain
- nervousness
- nightmares
- painful or difficult urination
- pinpoint red spots on the skin
- restless sleep
- seizures
- shakiness
- slurred speech
- sore throat
- unusual bleeding or bruising
- unusual tiredness or weakness
Rare
- Difficulty breathing or swallowing
- disturbed color perception
- double vision
- hives
- increased sweating
- muscle aches
- night blindness
- reddening of the skin, especially around ears
- ringing or buzzing in the ears
- swelling of the eyes, face, inside of the nose, fingers, feet, or lower legs
Incidence not known
- Back, leg, or stomach pains
- bleeding gums
- bleeding under the skin
- blindness
- blistering, peeling, or loosening of the skin
- bloody nose
- blue-yellow color blindness
- change in mental status
- chest pain
- cold sweats
- confusion
- cool, pale skin
- cough
- dark urine
- decreased frequency or amount of urine
- decreased vision
- depression
- diarrhea
- difficulty breathing
- difficulty in moving
- difficulty speaking
- dizziness
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- eye pain
- fainting
- fast, pounding, or irregular heartbeat or pulse
- general body swelling
- general feeling of discomfort, illness, or weakness
- hoarseness
- heavier menstrual periods
- hoarseness
- increased hunger
- increased or decreased urination
- increased sensitivity of the skin to sunlight
- increased thirst
- irregular heartbeat, recurrent
- irritation
- itching, skin rash
- joint pain, stiffness, or swelling
- light-colored stools
- loss of appetite
- muscle cramps, weakness, or stiffness
- nervousness
- nightmares
- nosebleeds
- painful or difficult urination
- pale color of the skin
- pale skin
- red skin lesions, often with a purple center
- red, irritated eyes
- redness or other discoloration of the skin
- severe
- sunburn
- sores, ulcers, or white spots in the mouth or on the lips
- tightness in the chest
- troubled swallowing
- upper right abdominal pain
- weakness
- weight gain
- yellow eyes or skin
Get emergency help immediately if any of the following symptoms of overdose occur while taking quinine:
Symptoms of an overdose
- Blindness
- blurred vision or change in vision
- chest pain
- dizziness
- double vision
- fainting
- lightheadedness
- rapid or irregular heartbeat
- sleepiness
Other side effects of Quinine
Some side effects of quinine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence not known
- Feeling of warmth
- heartburn
- lack or loss of strength
- pain or burning in the throat
- problems with speech or speaking
- restlessness
- thoughts or attempts of killing oneself tremors
- unsteadiness, trembling, or other problems with muscle control or coordination
- weight loss
For Healthcare Professionals
Applies to quinine: compounding powder, oral capsule, oral tablet.
General
This drug adversely affected almost all body systems. The most common side effects associated with this drug were a cluster of symptoms (cinchonism) which occurred to some degree in almost all patients using this drug.[Ref]
Hematologic
Disseminated intravascular coagulation has been reported in a 79-year-old female within 12 hours after a second 300 mg dose.[Ref]
Frequency not reported: Agranulocytosis, hypoprothrombinemia, thrombocytopenia (including fatal cases), hemolytic anemia, neutropenia, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, disseminated intravascular coagulation, idiopathic thrombocytopenic purpura, petechiae, ecchymosis, hemorrhage, coagulopathy, blackwater fever, leukopenia, pancytopenia, aplastic anemia, lupus anticoagulant, hemolysis (including acute), thrombocytopenic purpura, intravascular coagulation, immune thrombocytopenia, purpura[Ref]
Dermatologic
Frequency not reported: Cutaneous rashes (including urticarial, papular, scarlatinal), pruritus, bullous dermatitis, exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, rashes, fixed drug eruption (nummular skin lesion), photosensitivity reactions, allergic contact dermatitis, acral necrosis, cutaneous vasculitis (including fatal cases), urticaria, angioedema, eczematous dermatitis, erythema, lichen planus[Ref]
Fixed drug eruption (nummular skin lesion) has been reported in a 23-year-old female after exposure to quinine in tonic water. An open oral challenge (patient approved) with 30 mg quinine sulfate triggered the appearance of pruritus, erythema, and edema at the usual sites within 40 minutes of ingesting the dose.[Ref]
Gastrointestinal
Frequency not reported: Nausea, vomiting, diarrhea, abdominal pain, gastric irritation, esophagitis, epigastric pain, gastrointestinal upset[Ref]
Renal
Frequency not reported: Renal failure (including secondary to thrombotic thrombocytopenic purpura-hemolytic uremic syndrome), renal impairment/insufficiency, acute renal failure (due to immune mechanism or circulatory failure), acute interstitial nephritis, anuria, uremia, oliguria[Ref]
Respiratory
Frequency not reported: Asthma, dyspnea, pulmonary edema, asthma precipitation, asthmatic symptoms, bronchospasm, hemoptysis, transient bilateral pulmonary infiltrates[Ref]
Transient bilateral pulmonary infiltrates have been reported in a 45-year-old woman following a single 325 mg dose for nocturnal cramps. About 45 minutes after taking the dose, the following symptoms were present: sudden onset of dyspnea, wheezing, cough, breathlessness, severe anxiety, dry nonproductive cough, orthopnea, mild fever, chills, and pleuritic chest discomfort.[Ref]
Ocular
Frequency not reported: Diplopia, visual disturbances, blurred vision with scotomata, sudden loss of vision, photophobia, night blindness, diminished/constricted visual fields, fixed pupillary dilatation, disturbed color vision/perception, optic neuritis, blindness, mydriasis, optic atrophy, blurred vision, defective color perception, nystagmus[Ref]
Cardiovascular
Frequency not reported: Chest pain, vasodilatation, hypotension, tachycardia, bradycardia, palpitations, atrioventricular block, atrial fibrillation, irregular rhythm, unifocal premature ventricular contractions, nodal escape beats, U waves, QT prolongation, ventricular fibrillation, ventricular tachycardia, torsade de pointes, cardiac arrest, disturbance in cardiac rhythm/conduction, widening of QRS complex, angina symptoms, cardiovascular toxicity, atrioventricular conduction disturbances, fall in blood pressure with feeble pulse, T wave flattening, cardiac dysrhythmias[Ref]
Angina symptoms have been reported with prolonged therapy in sensitive patients.
Severe cardiovascular toxicity has been reported with rapid IV administration; fatal cases reported.[Ref]
Hepatic
Frequency not reported: Granulomatous hepatitis, hepatitis, jaundice, abnormal liver function tests, changes in the hepatic enzyme system that synthesizes vitamin K-dependent factors, hepatotoxicity, elevated alkaline phosphatase, elevated lactate dehydrogenase, elevated AST, elevated ALT, elevated GGT[Ref]
Within 24 hours of taking the first 260 mg dose for leg cramps, a 57-year-old Native American female presented to the hospital with symptoms of nausea, vomiting, generalized myalgia, headache, fever, chills, and rigor. The following liver enzymes were dramatically elevated: alkaline phosphatase, lactate dehydrogenase, AST, ALT, and GGT. After stopping this drug, the patient's symptoms resolved within 48 hours and the liver enzyme levels declined within 72 hours.[Ref]
Nervous system
Frequency not reported: Headache, seizures, coma, tremors, restlessness, ataxia, acute dystonic reaction, aphasia, syncope, vertigo, tinnitus, hearing impairment, deafness, loss of consciousness, dizziness, hearing loss[Ref]
Hypersensitivity
Frequency not reported: Hypersensitivity reactions (included asthma, angioneurotic edema, photosensitivity, hot and flushed skin, fever, pruritus, thrombocytopenic purpura, urticaria)[Ref]
Metabolic
Frequency not reported: Hypoglycemia, anorexia, hypoglycemia aggravated, electrolyte imbalance[Ref]
Other
Frequency not reported: Cinchonism (included deafness, tinnitus, headache, vasodilation and sweating, hearing impairment, rashes, vertigo/dizziness, blurred/disturbed vision, defective/disturbance in color perception, vomiting, diarrhea, abdominal pain, gastrointestinal symptoms, oculotoxicity, central nervous system disturbances, visual field constriction, blindness, nausea, disturbances in cardiac rhythm/conduction, cardiotoxicity, death), fever, chills, sweating, flushing, asthenia, facial edema, death, mucosal bleeding (gingival, gastrointestinal, epistaxis)[Ref]
Symptoms of mild cinchonism included headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo/dizziness, blurred vision, and disturbance in color perception; more severe symptoms of cinchonism were vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm/conduction. Most symptoms of cinchonism were reversible and resolved with discontinuation of this drug.[Ref]
Musculoskeletal
Frequency not reported: Lupus-like syndrome, myalgias, muscle weakness, myasthenia gravis aggravated, decreased neuromuscular transmission by increasing excitability threshold at myoneural junction, depressed muscle action potential
Psychiatric
Frequency not reported: Confusion, altered mental status, disorientation, suicide, apprehension, agitation
Genitourinary
Frequency not reported: Hemoglobinuria, abortion[Ref]
More about quinine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (20)
- Drug images
- Dosage information
- During pregnancy
- Drug class: antimalarial quinolines
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Cerner Multum, Inc. UK Summary of Product Characteristics.
2. Cerner Multum, Inc. Australian Product Information.
3. Blayney DW. Quinine-associated immune thrombopenia, neutropenia, and renal failure in a patient with Klinefelter's syndrome. Blood. 1992;10:2686.
4. Product Information. QuiNINE Sulfate (quiNINE). Zenith Goldline Pharmaceuticals. PROD.
5. Kedia RK, Wright AJ. Quinine-mediated disseminated intravascular coagulation. Postgrad Med J. 1999;75:429-30.
6. Chuah TL, Denaro C. A case of quinine-induced thrombocytopenia and neutropenia. Aust N Z J Med. 2000;30:96.
7. Brasic JR. Quinine-induced thrombocytopenia in a 64-year-old man who consumed tonic water to relieve nocturnal leg cramps. Mayo Clin Proc. 2001;76:863-4.
8. Kojouri K, Vesely SK, George JN. Summaries for patients. Quinine and thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Ann Intern Med. 2001;135:S-65.
9. Morton AP. Quinine-induced disseminated intravascular coagulation and haemolytic-uraemic syndrome. Med J Aust. 2002;176:351.
10. Asvadi P, Ahmadi Z, Chong BH. Drug induced thrombocytopenia: localization of the binding site of GPIX specific quinine-dependent antibodies. Blood. 2003.
11. Baliga RS, Wingo CS. Quinine Induced HUS-TTP: An Unusual Presentation. Am J Med Sci. 2003;326:378-80.
12. Reddy JC, Shuman MA, Aster RH. Quinine/Quinidine-induced thrombocytopenia: a great imitator. Arch Intern Med. 2004;164:218-20.
13. Bougie DW, Wilker PR, Aster RH. Patients with quinine-induced immune thrombocytopenia have both " drug-dependent " and " drug-specific " antibodies. Blood. 2006;108:922-7.
14. FDA Drug Safety Newsletter. Quinine (marketed as Qualaquin): overview of off-label use and serious adverse events. http://www.fda.gov/downloads/Drugs/DrugSafety/DrugSafetyNewsletter/UCM168579.pdf 2009.
15. In brief: safety of quinine. Med Lett Drugs Ther. 2010;52:88.
16. Asero R. Fixed drug eruptions caused by tonic water. J Allergy Clin Immunol. 2003;111:198-9.
17. Winstanley P. Malaria: treatment. J R Coll Physicians Lond. 1998;32:203-7.
18. Bakshi R, Hermeling-Fritz I, Gathmann I, Alteri E. An integrated assessment of the clinical safety of artemether-lumefantrine: a new oral fixed-dose combination antimalarial drug. Trans R Soc Trop Med Hyg. 2000;94:419-24.
19. Krantz MJ, Dart RC, Mehler PS. Transient pulmonary infiltrates possibly induced by quinine sulfate. Pharmacotherapy. 2002;22:775-8.
20. Feeney GFX, Lee GA, OConnor PA. Quinine-induced blindness during attempted heroin withdrawal. Med J Australia. 1999;170:449.
21. Farver DK, lavin MN. Quinine-induced hepatotoxicity. Ann Pharmacother. 1999;33:32-4.
22. White NJ, Pukrittayakamee S. Clinical malaria in the tropics. Med J Aust. 1993;159:197-203.
23. Vierira JL, Midio AF. Drug monitoring of quinine in men with nonsevere falciparum malaria: study in the Amazon region of Brazil. Ther Drug Monit. 2001;23:512-5.
24. Weinke T, Held T, Trautmann M, et al. Malaria therapy in 452 patients, with special reference to the use of quinine. J Infect. 1992;25:173-80.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.